4561
Left Ventricular Strain is associated with Outcomes of Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot
Baiyan Zhuang1, Minjie Lu1, and Shihua Zhao1
1Fuwai Hospital, State Key Laboratory of Cardiovascular Disease,PUMC, Beijing, China
1Fuwai Hospital, State Key Laboratory of Cardiovascular Disease,PUMC, Beijing, China
Synopsis
Given the fact that patients who have underwent repair of tetralogy of fallot (rTOF) further need pulmonary valve replacement (PVR) due to pulmonary regurgitation, but the effect of PVR is mixed. We prospectively enrolled 45 asymptomatic rTOF patients who required PVR due to moderate or severe pulmonary regurgitation and measured their pre-operative strain and strain rate. After follow-up and analysis, we found that the radial strain (RS), circumferential strain (CS), longitudinal strain (LS), systolic radial strain rate (RSRs), early diastolic radial strain rate (RSRe) and early diastolic longitudinal strain rate (LSRe) before PVR are important prognostic factors for adverse events.
Background:
Pulmonary valve replacement (PVR) is suitable and effective in reducing the right ventricular volume and retaining right ventricular function in patients with repaired tetralogy of Fallot (rTOF). However, prognostic outcomes after PVR surgery are still mixed. Key factors that determine outcomes after PVR in rTOF patients are largely unknown. Our study aims to analyze whether pre-PVR left ventricular strain and strain rate detected by cardiac magnetic resonance imaging (CMR) are associated with mid-term outcomes after PVR in patients with rTOF.
Method:
This prospective study enrolled 45 asymptomatic rTOF patients who required PVR due to moderate or severe pulmonary regurgitation. MR cine sequences were performed and the feature tracking parameters were measured pre-operatively(figure 1). Adverse events including death due to any causes, cardiac transplantation, application of implantable cardioverter defibrillator (ICD), symptomatic heart failure, syncope, reoperation for PVR, sustained atrial or ventricular arrhythmias and cardiac catheterization were documented during follow-up. ROC analysis was performed to obtain the cut-off value of pre-operative LV strain and strain rate for predicting adverse events. Kaplan-Meier curves were drawn with log-rank statistics and univariate and multivariate Cox's proportional hazards regression analyses were also analyzed.
Result:
During 3.2±1.6 years of follow-up, 12 adverse events were recorded. The 3-year event-free survival rate was 62% for patients with a pre-operative radial strain (RS)>29.25% (p<0.001), 47% for patients with a pre-operative circumferential strain (CS) <-14.3% (p<0.001), 66% for patients with a pre-operative longitudinal strain (LS) <-12.3% (p=0.014). As for strain rate, the 3-year event-free survival rate was 66% for patients with a pre-operative systolic radial strain rate (RSRs) >1.69s-1 (p=0.030), 70% for patients with a pre-operative early diastolic radial strain rate (RSRe) <-2.21 s-1 (p=0.021) and 62% for patients with a pre-operative early diastolic longitudinal strain rate (LSRe) >1.07 s-1 (p<0.001),(figure 2). After multivariate correction, LSRe was significantly associated with adverse outcomes (HR, 95% confidence interval: 0.012(0-0.956)).
Discussion and Conclusion:
The present study is the first to evaluate the predicting value of left strain parameters in rTOF patients after PVR surgery.The most important finding is: the left ventricular RS, CS, LS, RSRs, RSRe, LSRe before PVR are important prognostic factors for future events. Identifying these factors can help recognize patients at increased risk of adverse events.
Pulmonary valve replacement (PVR) is suitable and effective in reducing the right ventricular volume and retaining right ventricular function in patients with repaired tetralogy of Fallot (rTOF). However, prognostic outcomes after PVR surgery are still mixed. Key factors that determine outcomes after PVR in rTOF patients are largely unknown. Our study aims to analyze whether pre-PVR left ventricular strain and strain rate detected by cardiac magnetic resonance imaging (CMR) are associated with mid-term outcomes after PVR in patients with rTOF.
Method:
This prospective study enrolled 45 asymptomatic rTOF patients who required PVR due to moderate or severe pulmonary regurgitation. MR cine sequences were performed and the feature tracking parameters were measured pre-operatively(figure 1). Adverse events including death due to any causes, cardiac transplantation, application of implantable cardioverter defibrillator (ICD), symptomatic heart failure, syncope, reoperation for PVR, sustained atrial or ventricular arrhythmias and cardiac catheterization were documented during follow-up. ROC analysis was performed to obtain the cut-off value of pre-operative LV strain and strain rate for predicting adverse events. Kaplan-Meier curves were drawn with log-rank statistics and univariate and multivariate Cox's proportional hazards regression analyses were also analyzed.
Result:
During 3.2±1.6 years of follow-up, 12 adverse events were recorded. The 3-year event-free survival rate was 62% for patients with a pre-operative radial strain (RS)>29.25% (p<0.001), 47% for patients with a pre-operative circumferential strain (CS) <-14.3% (p<0.001), 66% for patients with a pre-operative longitudinal strain (LS) <-12.3% (p=0.014). As for strain rate, the 3-year event-free survival rate was 66% for patients with a pre-operative systolic radial strain rate (RSRs) >1.69s-1 (p=0.030), 70% for patients with a pre-operative early diastolic radial strain rate (RSRe) <-2.21 s-1 (p=0.021) and 62% for patients with a pre-operative early diastolic longitudinal strain rate (LSRe) >1.07 s-1 (p<0.001),(figure 2). After multivariate correction, LSRe was significantly associated with adverse outcomes (HR, 95% confidence interval: 0.012(0-0.956)).
Discussion and Conclusion:
The present study is the first to evaluate the predicting value of left strain parameters in rTOF patients after PVR surgery.The most important finding is: the left ventricular RS, CS, LS, RSRs, RSRe, LSRe before PVR are important prognostic factors for future events. Identifying these factors can help recognize patients at increased risk of adverse events.
Acknowledgements
noneReferences
noneFigures
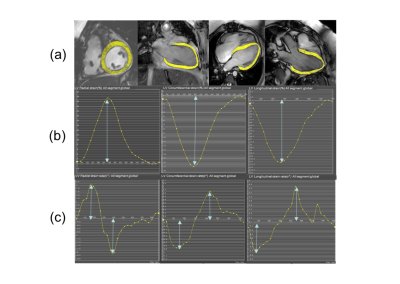
Representative short-axis and long-axis images
(a), strain (b) and strain rate curves (c) in a subject underwent pulmonary
valve replacement (PVR). The epicardial and endocardial borders (excluding
papillary muscles and trabeculae) at end-diastole were semi-manually defined on
the LV 4 chamber, LV 2 chamber and LV 3 chamber to calculate longitudinal stain
and strain rate. The entire LV short-axis SSFP cine images were used to
calculate radial and circumferential stain and strain rate.
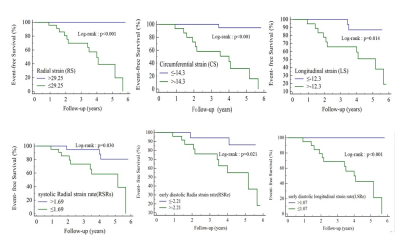
Figure 2. Kaplan-Meier survival
curves for patient subgroups stratified by peak radial strain(RS), peak
circumferential strain(CS), peak longitudinal strain(LS), peak systole radial
strain rate (RSRs), peak early diastole radial strain rate (RSRe) , peak circumferential
strain rate at end-diastole(CSRe) and peak early diastole longitudinal strain
rate(LSRe).
DOI: https://doi.org/10.58530/2022/4561