4557
Evaluation of cardiotoxicity in chest tumor patients receiving immune checkpoint inhibitors by cardiovascular magnetic resonance1wuhan union hospital, wuhan, China, 2wuhan tongji hospital, wuhan, China, 3Siemens Healthcare, shanghai, China
Synopsis
In our study, we conducted a prospective study to investigate the subclinical cardiotoxicity by serial cardiovascular magnetic resonance (CMR) in patients receiving immune checkpoint inhibitor (ICI). Some functional parameters and global strains of bi-ventricles revealed significant decrease at the early stage on ICI therapy, and ejection fraction as well as global strain values of both ventricles all showed a decline trend. Tissue characterization is an extra advantage of CMR technique. While in our study, parameters (T1 mapping, T2 mapping and late gadolinium enhancement) regarding tissue characterization of global myocardium showed no significant differences, compared with baseline data.
Introduction
Limited data exists on the subclinical effects of cardiotoxicity in chest tumor patients receiving immune checkpoint inhibitors (ICIs) [1-3]. Therefore, we aimed to evaluate the manifestations of subclinical cardiotoxicity in this patient cohort using cardiovascular magnetic resonance (CMR), and their relationship with baseline CMR and clinical parameters.Method
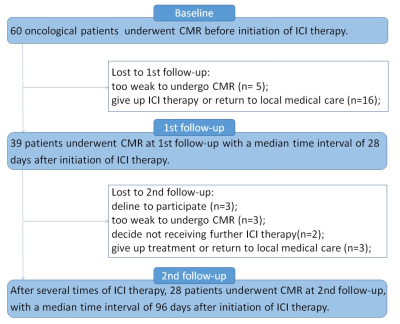
A prospective, longitudinal study was conducted in chest tumor patients (n = 60). Following informed consent, patients underwent serial CMR (1.5T scanner, MAGNETOM Altea, Siemens Healthineers, Erlangen, Germany) at three time points: baseline, 3 weeks (1st follow-up), and 3 months (2nd follow-up) after initiation of ICI therapy (Figure 1). Patients who underwent at least 2 CMR examinations (baseline and 1st follow-up CMR data) were included in the analysis. The following CMR parameters were assessed: functional parameters and global strains of left ventricle (LV) and right ventricle (RV), T1 mapping and derived extracellular volume fraction (ECV), and T2 mapping and late gadolinium enhancement (LGE). According to the recent task force criteria [4-5], an LV ejection fraction (LVEF) with a > 10% decrease compared with baseline LVEF was defined as reduced LVEF, while a reduced RV ejection fraction (RVEF) was defined as < 45%.Results
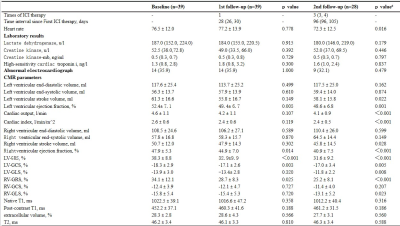
Thirty-nine patients (n = 39, age = 60.3 ± 10.0 years, 28 males) successfully underwent baseline and first follow-up CMR. Of these, 24 (61.5%) had at least one risk factor. Most patients (92.3%) had lung cancer, and all patients received ICI monotherapy. Compared with baseline data, LVEF, RVEF, LV global radial strain and circumferential strain, and RV global radial strain showed significant decrease at 1st follow-up (Figure 2, Table 1). There were 28 patients (age = 60.3 ± 9.3 years, 21 males) with CMR data at 2nd follow-up, and LVEF, RVEF, and global strains of both ventricles showed further reduction. Native T1, post-contrast T1, ECV, and T2 values revealed no statistically significant differences (p > 0.05). The presence of CV risk factor represented a predictor of LVEF reduction > 10% at 1st follow-up (p = 0.020). A baseline LVEF < 53% emerged as significant for predicting both reduction of LVEF > 10% (p = 0.030) and RVEF < 45% (p = 0.040) at 2nd follow-up.Conclusion
At the early stage of ICI therapy, bi-ventricular dysfunction is the main manifestation of subclinical myocardial injury in patients with chest tumors. A baseline LVEF < 53% may be associated with further reduction in bi-ventricular dysfunction in this patient population.Acknowledgements
Not applicable.References
1. Saunderson CE, Plein S, Manisty CH. Role of cardiovascular magnetic resonance imaging in cardio-oncology. Eur Heart J Cardiovasc Imaging. 2021;22:383-96.
2. Higgins AY, Arbune A1, Soufer A, Ragheb E, Kwan JM, Lamy J, et al. Left ventricular myocardial strain and tissue characterization by cardiac magnetic resonance imaging in immune checkpoint inhibitor associated cardiotoxicity. PLoS One. 2021;16:e0246764.
3. Zhang L, Awadalla M, Mahmood SS, Nohria A, Hassan MZ, Thuny F, et al. Cardiovascular magnetic resonance in immunecheckpoint inhibitor-associated myocarditis. Eur Heart J. 2020;41:1733–43.
4. Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Crosbie MS, ET al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27:911-39.
5. Etoom Y, Govindapillai S, Hamilton R, Manlhiot C, Yoo SJ, Farhan M, et al. Importance of CMR within the Task Force Criteria for the diagnosis of ARVC in children and adolescents. J Am Coll Cardiol. 2015;65:987-95.
Figures