4551
Left ventricular blood flow kinetic energy in Hypertensive heart disease :A pilot study of 4D flow cardiovascular magnetic resonance1Department of Radiology, Shanghai Tenth People’s Hospital, School of Medicine,Tongji University, Shanghai, China, 2Department of Cardiology, Shanghai Tenth People’s Hospital, School of Medicine,Tongji University, Shanghai, China, 3Philips Healthcare, Shanghai, China
Synopsis
Four-dimensional flow magnetic resonance imaging (4D-flow MRI) technique has been developed to assess intra-cavity left ventricular (LV) blood flow. Hypertensive heart disease (HHD) is a common cardiovascular disease and manifested as left ventricular hypertrophy and diastolic/systolic dysfunction. The purpose of this study was to investigate whether 4D-flow CMR kinetic energy (KE) parameters are sensitive to distinguish HHD patients from age/gender-matched healthy controls, and to access if there are significant differences in different sub-groups of LV ejection fraction. We also aimed to investigate the association of LV KE to LV function parameters and LV mass.
Introduction
Hypertensive heart disease (HHD) is a common cardiovascular disease [1] . HHD patients are prone to left ventricular(LV)diastolic dysfunction before left ventricular hypertrophy and impaired LV systolic function[2]. Both systolic and diastolic dysfunction can cause hemodynamic changes. Therefore, the assessment of LV hemodynamics may provide incremental value in patients with HHD.The developed four-dimensional flow cardiovascular magnetic resonance (4D-flow CMR) now allows quantification of intra-cavity flow kinetic energy (KE), which can help capture intra-cardiac flow and offer novel insights into complex flow patterns associated with LV circulation [3, 4] . Previous studies revealed that the LV peak E-wave declined with aging[5]. Another study demonstrated that LV systolic average KE was higher in patients with heart failure compared to healthy controls, but lower when indexed to end diastolic volume [6]. And in dilated cardiomyopathy, even though the stroke volume remained equal to healthy controls,the lower efficiency of blood flow patterns were observed[7]. At present, it is unclear if abnormal LV KE can be seen in HHD.
The purpose of this study was as follows: 1) to quantify dynamic parameters of LV blood flow KE in HHD patients and age/gender-matched healthy controls; 2) to investigate if there are significant differences in LV blood flow KE in different sub-groups of LV ejection fraction(LV EF); 3) to investigate the association of LV KE to LV function parameters and LV mass.
Methods
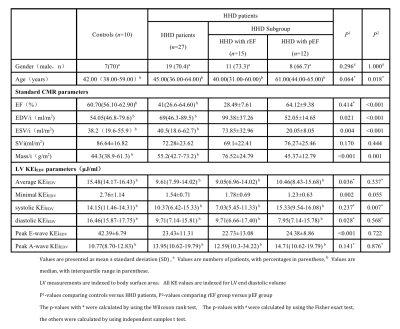
Population characteristics:Twenty-seven HHD patients and ten age/gender-matched healthy controls were included. HHD patients were divided into the preserved ejection fraction(pEF,EF≥50%)group (n =12) and reduced ejection fraction(rEF,EF<50%)group (n = 15).MR sequence:All subjects were imaged on an Ingenia CX 3.0T MR system.
Balanced steady-state free precession(bSSFP) cine images were acquired during repeated end-expiratory breath holds. Typical parameters for bSSFP cine were as follows: SENSE factor=2, flip angle=60°, repetition time (TR) /echo time (TE) = 1.5/3 ms, field of view (FOV) = 320–420 mm according to patient size, slice thickness = 8 mm, and 30 phases per cardiac cycle.
For 4D flow, Compressed-SENSE(C-SENSE) accelerated 4D flow sequence was used, with retrospective ECG triggering and a C-SENSE factor at 8. 4D flow was acquired during free breathing with respiratory gating and the field of view covered the entire heart by transversal plane. Typical scanning parameters were TE/TR = 3.7/6.2 ms, flip angle = 8°, acquired and reconstructed voxel size = 3x3x3 mm3, VENC =150 cm/s. The acquired temporal resolution was typically 50–55 ms, rendering 10–21 phases depending on heart rate, and the result was reconstructed to 30 heart phases.
Image analysis:All images were analyzed by two expert radiologists who were blinded to clinical results. CMR cine images and 4D flow data were evaluated by offline research software (MASS; Version 2016 EXP, Leiden University Medical Center, Leiden, The Netherlands). Standard CMR parameters included: end diastolic volume (EDV), end systolic volume (ESV), SV (stroke volume), ejection fraction (EF) and LV mass index. LV blood flow KE parameters were indexed to LV EDV and included: averaged LV, minimal KEiEDV, systolic KEiEDV, diastolic KEiEDV, peak E-wave and peak A-wave KEiEDV.
Statistical analysis :Standard CMR parameters and KE parameters between groups were compared by using independent samples t-test or Wilcoxon rank test. Association between KE parameters and standard CMR parameters was accessed by Pearson or Spearman’s correlation test.
Results
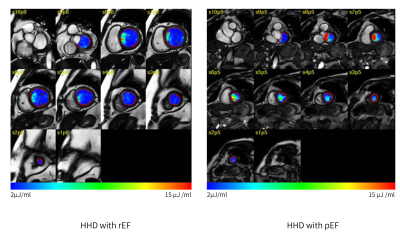
1)LV average KEiEDV was higher in controls than that of HHD patients [15.48(14.17-16.43) μJ/ml versus 9.61(7.59-14.02) μJ/ml, P = 0.036]. Additionally,minimal, diastolic and peak E-wave KEiEDV were lower in HHD patients than those of controls(P < 0.05) (table 1).2)In HHD patients with rEF, the systolic KEiEDV were lower than HHD patients with pEF [7.03(5.45-11.33) μJ/ml versus 15.33(9.54-16.08) μJ/ml, P = 0.007](Fig 1).
3)In correlation analysis, minimal KEiEDV demonstrated the significant correlation with the EDV and LV mass index in all groups (r=0.524, P=0.007; r=0.681, P<0.001).
Discussion
In the present study, the average KEiEDV , in essence is the global density of the velocity profile of intra-cavity blood flow, was significantly lower in patients with HHD than controls. The reduction in diastolic and peak E-wave KEiEDV in HHD patients demonstrated that HHD was accompanied by diastolic dysfunction.In the comparison between pEF and rEF, the systolic KEiEDV was lower in rEF group, which was a consequence of global hypo-contractility. It results in lower pressure gradient between the LV and the aorta,and the reduction of the overall thrust of systolic blood flow.
The minimal KEiEDV correlated with EDV and LV mass index significantly. This parameter represents the minimal KE of the LV flow throughout all phases of the cardiac cycle. It is likely to occur when the hemodynamic forces are minimal and LV flow is not exist. We suspected that left ventricular mass index and EDV increased with the progression of HHD, which may lead to the loss of LV systolic mechanical thrust and restrictive diastolic filling.
Conclusion
Reductions were observed in average KEiEDV, minimal KEiEDV, diastolic KEiEDV and peak E-wave KEiEDV in HHD patients. There was a significant decrease of LV systolic KEiEDV in HHD patients with rEF. And the minimal KEiEDV was significant correlated with the progression of HHD. These KE parameters may offer novel mechanistic insights to describe and research the hemodynamics changes in HHD patients.Acknowledgements
This work is supported by grants from National Natural Science Foundation of China [No 81871325], Project of STCSM[20Y11911899].
References
1. Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39:3021–31042.
2. Marijana Tadic , Cesare Cuspidi , Sven Plein et al. Comprehensive assessment of hypertensive heart disease: cardiac magnetic resonance in focus. Heart Fail Rev. 2021 Nov;26(6):1383-1390.
3. Harjinder Kaur , Hosamadin Assadi , Samer Alabed et al. Left Ventricular Blood Flow Kinetic Energy Assessment by 4D Flow Cardiovascular Magnetic Resonance: A Systematic Review of the Clinical Relevance. J Cardiovasc Dev Dis. 2020 Sep 10;7(3):37.
4. Rob J van der Geest , Pankaj Garg . Advanced Analysis Techniques for Intra-cardiac Flow Evaluation from 4D Flow MRI. Curr Radiol Rep. 2016;4:38.
5. Daniela Föll , Steffen Taeger, Christoph Bode. Age, gender, blood pressure, and ventricular geometry influence normal 3D blood flow characteristics in the left heart. Eur Heart J Cardiovasc Imaging. 2013 Apr;14(4):366-73.
6. Mikael Kanski , Per M Arvidsson , Johannes Töger et al. Left ventricular fluid kinetic energy time curves in heart failure from cardiovascular magnetic resonance 4D flow data. J Cardiovasc Magn Reson. 2015 Dec 20;17:111.
7. Jonatan Eriksson , Ann F Bolger, Tino Ebbers, Carl-Johan Carlhäll et al. Four-dimensional blood flow-specific markers of LV dysfunction in dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2013 May;14(5):417-24.