4545
Severe Cerebral Small Vessel Disease Burden is Associated with Brain Hypo-perfusion, and higher Framingham Risk score: An 8 year follow-up study1Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2State Key Laboratory of Brain and Cognitive Science, Institute of Biophysics, Chinese Academy of Sciences, Beijing, China, 3Department of Human Anatomy, Histology and Embryology, School of Basic Medicine, Peking Union Medical College, Beijing, China
Synopsis
The study investigated
relationship between cerebral small vessel disease (CSVD) burden, cerebral
blood flow (CBF) and cardiovascular risk in the aging brains with normal
cognitive function at baseline and conducted telephone cognitive follow-up for
nearly 8 years. The results showed that severe CSVD burden was significantly
associated with higher cardiovascular risk scores and decreased CBF in multiple
areas, with
involvement of nearly all cortical brain areas. Subjects with severe CSVD
burden were more likely to suffer from long-term cognitive decline. This suggests
the capability of CSVD burden serving as an imaging marker of predicting
cognitive decline.
Introduction/Purpose
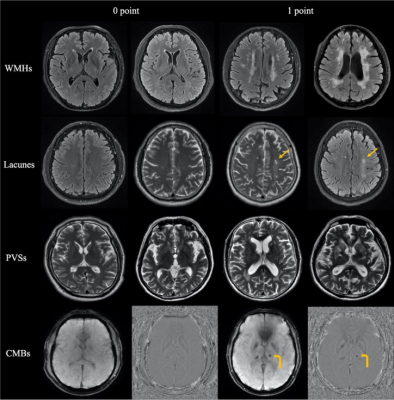
Cerebral small vessel disease (CSVD) is a common age-related vascular disease of the brain which is often insidious in its onset[1]. At present, total CSVD burden score including hyperintensity(WMH), lacune, cerebral microbleeds (CMBs), and perivascular spaces (PVS) is a commonly used method to evaluate the severity of the disease[2]. Accumulating evidence has shown that CSVD patients experienced global alterations in brain structure and perfusion and the severity is associated with cognitive decline[3; 4]. The majority of studies have focused on an individual cerebral small vessel imaging marker, ignoring their sequential or co-occurring relationship. However, their significance in an aging brain remains poorly understood. Here, we investigated their relationship with gray matter cerebral blood flow (CBF) in the aging brain in a large sample of cognitively intact older adults.Methods
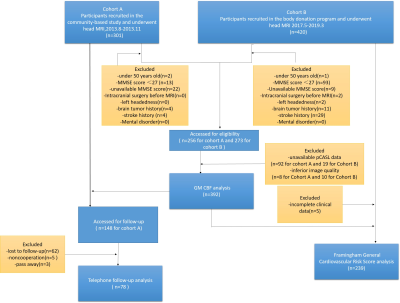
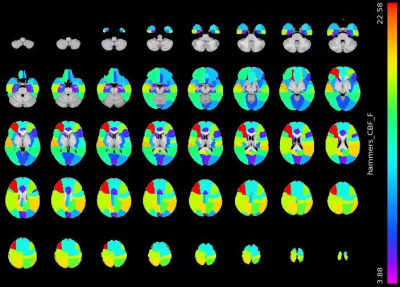
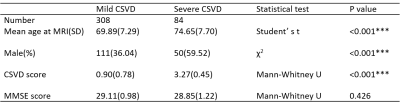
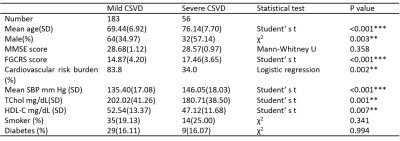
A total of 721 volunteers were recruited. Figure 1 shows the flowchart of participant enrollment. MRI was performed with 3.0 T MRI scanner (GE Discovery MR750,GE Healtchare, Milwaukee, WI, United States)using a pseudo-continuous arterial spin labeling (pCASL) sequence and a sagittal isotropic T1-weighted sequence for CBF analysis. The images obtained from MR images obtained from 392 participants whose MMSE scores ≥27 were used to investigate the relationship between the severity of CSVD and CBF. All four MRI markers of CSVD (lacunes, WMHs, PVSs, and CMBs) were identified from conventional brain sequences according to the previously reported neuroimaging standards[2]. Seventy-eight participants completed a telephone survey regarding cognitive function 7.6 years (± 0.1 years) after undergoing MRI. The survey evaluated their cognitive performance using the Subjective Cognitive Decline-Questionnaire 9[5] and their clinical history. CSVD scores were rated using a 5-grade score from 0 to 4. The severity of CSVD was classified as mild (grade≤2) and severe (grade>2). Cardiovascular risk burden was assessed with the Framingham General Cardiovascular Risk Score (FGCRS)[6], We calculated FGCRS based on age, sex, high-density lipoprotein cholesterol, total cholesterol, systolic blood pressure (SBP),diabetes, and smoking history[7]. FGCRS is calculated by summing up the points from all of these risk factors, and the cardiovascular risk burden was divided into two categories for statistical analysis, lower (FGCRS<17) and higher (FGCRS≥17)[8]. The difference in CBF between the mild and severe CSVD group was compared using univariate linear analysis, and logistic regression analysis was performed to assess the risk of longitudinal cognitive function and cardiovascular risk.Results
Severe CSVD burdens were significantly associated with higher cardiovascular risk score (P=0.002) at baseline and smaller CBF in multiple cortical regions and some deep nucleus (PFDR< 0.05, corrected for GMV, age and sex). Compared with participants with mild CSVD, participants with severe CSVD were more susceptible to longitudinal cognitive decline (OR= 3.375, 95%CI = [1.628, 6.995], p= 0.001, corrected for age, sex, education years, and MMSE).Discussion
To explore preventative methods for cognitive decline, it is essential to recognize risk at individual years before the onset of clinical symptoms. The results of this study indicate that in cognitively intact older adults, severe CSVD burdens are associated with brain hypo-perfusion at baseline. And participants with severe CSVD burdens are more susceptible to longitudinal cognitive decline. Early detection and improvement of vascular risk factors such as total cholesterol and hypertension in aging as well as regular follow-up of CSVD burden has the potential to reduce the risk of developing cognitive decline.Conclusions
Severe CSVD burden, which is associated with smaller CBF and higher cardiovascular risk score, serves as an imaging marker of predicting cognitive decline.Acknowledgements
We sincerely thank the participants in this study.References
[1] D. Pinter, C. Enzinger, and F. Fazekas, Cerebral small vessel disease, cognitive reserve and cognitive dysfunction. Journal of neurology 262 (2015) 2411-9.
[2] J. Wardlaw, E. Smith, G. Biessels, C. Cordonnier, F. Fazekas, R. Frayne, R. Lindley, J. O'Brien, F. Barkhof, O. Benavente, S. Black, C. Brayne, M. Breteler, H. Chabriat, C. Decarli, F. de Leeuw, F. Doubal, M. Duering, N. Fox, S. Greenberg, V. Hachinski, I. Kilimann, V. Mok, R. Oostenbrugge, L. Pantoni, O. Speck, B. Stephan, S. Teipel, A. Viswanathan, D. Werring, C. Chen, C. Smith, M. van Buchem, B. Norrving, P. Gorelick, M. Dichgans, and J.T.L.N. , Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. 12 (2013) 822-38.
[3] C. Yu, W. Lu, J. Qiu, F. Wang, J. Li, and L. Wang, Alterations of the Whole Cerebral Blood Flow in Patients With Different Total Cerebral Small Vessel Disease Burden. Front Aging Neurosci 12 (2020) 175.
[4] X. Xu, K.K. Lau, Y.K. Wong, H.K.F. Mak, and E.S. Hui, The effect of the total small vessel disease burden on the structural brain network. Sci Rep 8 (2018) 7442.
[5] S.H. Lee, Y. Kang, and S.J. Cho, Subjective cognitive decline in patients with migraine and its relationship with depression, anxiety, and sleep quality. The journal of headache and pain 18 (2017) 77.
[6] C. Iadecola, and N.S. Parikh, Framingham General Cardiovascular Risk Score and Cognitive Impairment: The Power of Foresight. Journal of the American College of Cardiology 75 (2020) 2535-2537.
[7] R.B. D'Agostino, Sr., R.S. Vasan, M.J. Pencina, P.A. Wolf, M. Cobain, J.M. Massaro, and W.B. Kannel, General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 117 (2008) 743-53.
[8] R. Song, H. Xu, C.S. Dintica, K.Y. Pan, X. Qi, A.S. Buchman, D.A. Bennett, and W. Xu, Associations Between Cardiovascular Risk, Structural Brain Changes, and Cognitive Decline. Journal of the American College of Cardiology 75 (2020) 2525-2534.
Figures