4543
Reference value of ascending aorta global longitudinal strain by cardiovascular magnetic resonance feature tracking1National Heart Centre Singapore, Singapore, Singapore, 2Department of Cardiovascular Medicine, The Second Affiliated Hospital of Nanchang University, Nanchang, China, 3Duke-NUS Medical School, Singapore, Singapore, 4National University Heart Centre, Singapore, Singapore, 5Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore, 6National University Hospital, Singapore, Singapore
Synopsis
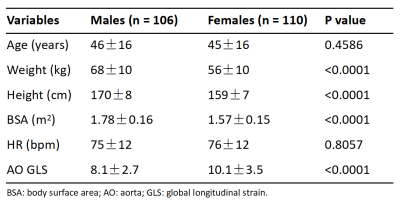
This study aimed to introduce a novel parameter—aorta (AO) global longitudinal strain (GLS)—for AO stiffness assessment by semi-automated feature tracking approach with standard cine cardiovascular magnetic resonance (CMR). The data demonstrated excellent intra and inter-observer variability of AO GLS of 4.4% and 5.0%, respectively. AO GLS was significantly negatively associated with age. The mean AO GLS was greater in females (10.1±3.5% versus 8.1±2.7%, P<0.001). The AO GLS decreased by 1.68% in females and 1.32% in males per decade respectively. Age was an independent predictor of the AO GLS in both males and females.
Background and Purpose
Aortic stiffness increases with age, as well as in various cardiovascular risk factors, including obesity, hypertension, diabetes mellitus, dyslipidemia, and smoking1,2, and it has been a hallmark of aging. The ascending aortic longitudinal strain negatively correlated with aortic stiffness3-5. In this study, we proposed a novel parameter—aorta (AO) global longitudinal strain (GLS)—to quantify the AO stiffness using a semi-automated strain measurement approach with standard cine cardiovascular magnetic resonance (CMR) images. Second, we aimed to establish reference values of AO GLS.Methods
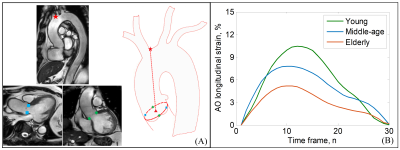
216 healthy participants (21 to 79 years old, 110 Females) from 2 centers with CMR scans were enrolled. Subjects who had physician-diagnosed cardiovascular diseases (such as coronary heart disease, atrial fibrillation and stroke) or cardiovascular risk factors (obesity, hypertension, diabetes mellitus, dyslipidemia and ever smoked) were excluded. The CMR scans for all subjects were imaged using a 3T magnetic resonance imaging system or 1.5T system (MAGNETOM Aera, Siemens Healthineers). Standard end-expiratory breath-hold cine images (steady-state free precession pulse sequence, retrospective electrocardiographic gating, typical temporal resolution 30 frames per cardiac cycle) were acquired in the Arch, left ventricular outflow tract (LVOT), and coronal LVOT views (Figure 1). We used an in-house semi-automatic algorithm to track the origin of the brachiocephalic artery from the aorta, and the aortic valve annulus in three-dimensional (3D) space: (1) landmarks on the artery origin (red star) and aortic valve annulus (two blue squares and two green diamonds) were automatically tracked over the cardiac cycle (Figure 1A), (2) the trajectory of the centroid was derived from four aortic annular points, (3) the distance (L) between the artery origin and centroid was calculated, (4) longitudinal strain at a time point (t) relative to the initial time point (time 0) at end-diastole was calculated as $$$\frac{(L(t)-L(0))*100}{L(0)}$$$, and (5) the AO GLS was defined as the maximal absolute strain value (Figure 1B).Results
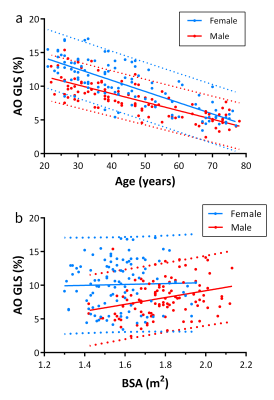
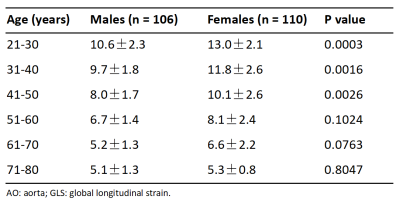
The AO GLS was successfully assessed in all subjects. The age was comparable in females and males (45±16 versus 46±16 years, P=NS). The BSA was different between females and males (1.57±0.15 versus 1.78±0.16 m2, P<0.001). The mean AO GLS was greater in females (10.1±3.5% versus 8.1±2.7%, P<0.001) (Table 1). All participants were stratified into six groups by age. The differences of AO GLS between females and males were mainly occurred in participants younger than 50 years old (all P<0.01) (Table 2). The AO GLS decreased with age but increased with BSA (Figure 2). Age was correlated significantly with AO GLS in both females and males (R2=0.611 and 0.602, respectively; both P<0.0001). Among males, BSA was associated with AO GLS (P=0.0022) but the R2 value was low (0.087), which was not the case among females. In multivariate regression analysis, age was significantly negatively associated with the AO GLS in females and males (R2=0.616 versus R2=0.610, both P<0.0001). The AO GLS decreased by 1.68% in females and 1.32% in males per decade respectively. The intra and inter-observer variability of AO GLS were 4.4% and 5.0%, respectively.Conclusion
We have demonstrated that measurement of the AO GLS parameter from cine CMR is feasible. This will be a novel radiographic parameter for quantitation of aortic stiffness. Age was an independent predictor of the AO GLS in both males and females. The AO GLS in females was significantly greater than males under 50 years old.Acknowledgements
No acknowledgement found.References
1. Miyoshi T, Ito H. Arterial stiffness in health and disease: The role of cardio-ankle vascular index. J Cardiol 2021;78:493-501.
2. Bell V, Mitchell WA, Sigurethsson S, et al. Longitudinal and circumferential strain of the proximal aorta. Journal of the American Heart Association 2014;3:e001536.
3. Guala A, Teixido-Tura G, Rodriguez-Palomares J, et al. Proximal aorta longitudinal strain predicts aortic root dilation rate and aortic events in Marfan syndrome. Eur Heart J 2019;40:2047-55.
4. Wu J, Pei Y, Wang Y, et al. Evaluation of Ascending Aortic Longitudinal Strain Via Two-Dimensional Speckle Tracking Echocardiography in Hypertensive Patients Complicated by Type A Aortic Dissection. J Ultrasound Med 2021.
5. Plonek T, Berezowski M, Kurcz J, et al. The evaluation of the aortic annulus displacement during cardiac cycle using magnetic resonance imaging. BMC cardiovascular disorders 2018;18:154.
Figures