4534
To assess the patients with brachial plexus injury and the changes of T2 value after injury by using T2 mapping1Philips Healthcare, Beijing, China, 2The Third Hospital of Hebei Medical University, Shijiazhuang, China
Synopsis
T2 mapping can provide quantitative parameter T2 values without radiation and damage, which can be used to quantitatively evaluate tissue inflammation and edema. The aim of this study was to evaluate patients with brachial plexus injury by using T2 mapping. And results showed that the T2 value would be prolonged when brachial plexus injured, and the T2 value would be shortened as patients recovers.
Introduction
The evaluation of prognosis is different due to the position and degree of the injury when the patients with brachial plexus injury. The conventional magnetic resonance imaging (MRI) method for patients with brachial plexus injury is to evaluate the morphology and signal size, which lacks quantitative and objective results1. T2 mapping is a non-radiation and non-invasive technique that can be used to calculate values of spin-spin or transverse relaxation of tissue and has been widely used to evaluate myocardial inflammation and edema2-4. In previous studies, the rabbit model of unilateral sciatic nerve stretch was established, and the T2 values and recovery of disorderly injured sites in different phases were compared5. But there were few studies paid attention to the application of T2 mapping on patients with brachial plexus injury. Therefore, the purpose of this study was to prospectively evaluate the clinical feasibility of T2 mapping in patients with brachial plexus injury, and to evaluate the relationship for the changes in T2 values preliminary in difference phases.Methods
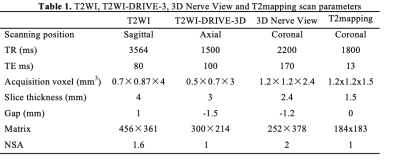
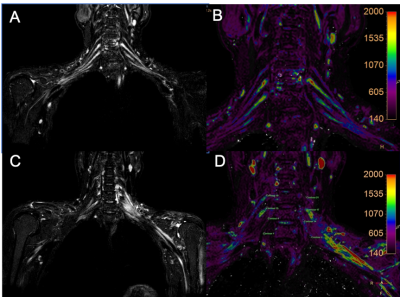
Healthy volunteers and patients with brachial plexus injury for different lengths of time after injury were performed on a 3.0T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands). The scan sequences included T2 weighted(T2WI), T2WI-DRIVE-3D, 3D Nerve View and T2 mapping. More information of sequences was listed in Table 1. The post-processing process is as follows: Firstly, imagings were processed by using Philips’s workstation (ISP, Philips Healthcare, the Netherlands). Fusion of T2WI-DRIVE-3D and T2 mapping to identify the location of region of interest (ROI) by an experienced radiologist (with 3-year experience). Secondly, the T2 value of the corresponding position were obtained. Finally, T2 values between patients with different injury durations, and between patients and healthy volunteers were comparedResults
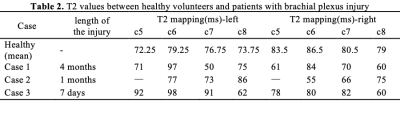
4 healthy volunteers and 3 patients with brachial plexus injury were enrolled in this study (the value of T2 cannot be measured because of metal implant for case 2). T2 mean values of different nerves were calculated in the healthy group as shown in Table 2. And the length of time for patients who underwent MRI examination after left injury was 4 months, 1 months and 7 days. For healthy volunteers, the T2 value of the right nerve was higher than that in the left, which had similar trend with patients in the 4-month group as shown in Figure 1. Furthermore, with the extension of time after injury, the T2 value of patients was more similar to that of healthy volunteers.Discussion
In this article, the data currently available were used to analyze the relationship between T2 values and patients. The results showed that for patients, the T2 value would increase when the brachial plexus was injured, which was consistent with the trend of previous animal models5. More importantly, the T2 value would gradually decrease to a value similar to that of healthy volunteers with treatment and recovery. We speculate that this may be due to a decrease in inflammation or edema, which would restore the T2 value to the normal level. This means that the use of T2 mapping technique may provide effective information for prognostic evaluation of patients with brachial plexus injury. Furthermore, it is necessary to collect more data to further verify our conclusions.Conclusion
T2 mapping may provide an effective method for the evaluation of patients with brachial plexus injury, and may be a promising way to assess difference phases.Acknowledgements
No acknowledgement.References
1. Hiwatashi A, Togao O, Yamashita K, et al. Simultaneous MR neurography and apparent T2 mapping in brachial plexus: Evaluation of patients with chronic inflammatory demyelinating polyradiculoneuropathy. Magn Reson Imaging. 2019;55:112-117.
2. Luetkens JA, Klein S, Träber F, et al. Quantification of Liver Fibrosis at T1 and T2 Mapping with Extracellular Volume Fraction MRI: Preclinical Results. Radiology. 2018;288(3):748-754.
3. Sollmann N, Weidlich D, Cervantes B, et al. T2 mapping of lumbosacral nerves in patients suffering from unilateral radicular pain due to degenerative disc disease. J Neurosurg Spine. 2019;1-9.
4. Eguchi Y, Enomoto K, Sato T, et al. Simultaneous MR neurography and apparent T2 mapping of cervical nerve roots before microendoscopic surgery to treat patient with radiculopathy due to cervical disc herniation: Preliminary results.
5. Shen J, Zhou CP, Zhong XM, et al. MR neurography: T1 and T2 measurements in acute peripheral nerve traction injury in rabbits. Radiology. 2010;254(3):729-738.
Figures