4532
Quantitative assessment of lumbar nerve root compression using contrast-enhanced 3D-FIESTA imaging sequence1First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha, China, 2GE Healthcare, Beijing, China
Synopsis
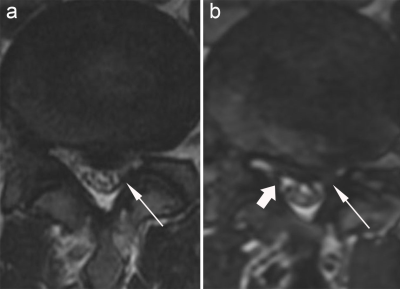
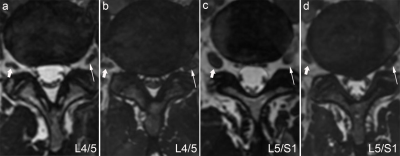
Actual contact surface between the extraforaminal nerve root and the adjacent structures is commonly missing on the conventional MR scanning, possibly leading to misdiagnosis. In our study, the detection rate of nerve root compression was significantly higher on the 3D-FIESTA-C images than T2WI. The shortest distance between the extraforaminal nerve root and the disc of L4/5 and L5/S1 in the healthy group was significantly longer than that in the lumbar disc herniation (LDH) group. The spatial relationship between nerve roots and surrounding tissues could be better described using 3D-FIESTA-C sequence and was helpful for the detection of nerve root compression.
Introduction
Lumbar disc herniation (LDH) is a common disease in orthopedics. After the degenerative changes of the lumbar intervertebral disc, the nucleus pulposus of the intervertebral disc protrudes from the ruptured annulus fibrosus under the action of external force, and the adjacent spinal nerve roots are stimulated or compressed,1-2 which results in low-back pain as well as numbness. To detect intervertebral disc lesions using magnetic resonance imaging (MRI) is common.3 However, due to partial volume artifacts and limitation of layer thickness, the actual contact surface between nerve root and disc may be missed on routine sequences.4-5 It is also difficult to show the distal lateral lumbar disc herniation using routine sequences in the sagittal view 6-7. This study aimed to explore the diagnostic performance of contrast-enhanced three-dimensional fast imaging employing steady-state acquisition (3D-FIESTA-C) imaging sequence on the lumbar nerve roots and to measure the geometric parameters between lumbar nerve roots and adjacent tissues.Material and methods
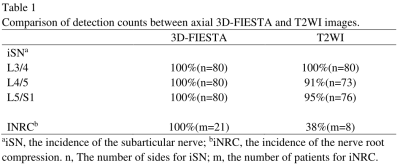
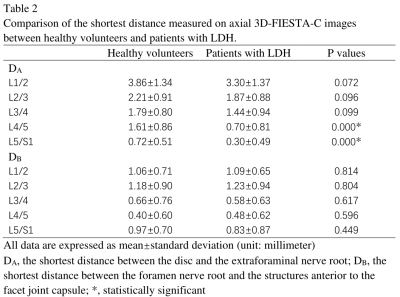
19 healthy volunteers and 21 patients with LDH underwent lumbar spine examination using routine MRI and 3D-FIESTA imaging on a 3.0-T MR scanner (Signa HDxt, GE Healthcare). The original 3D-FIESTA images were post-processed to generate the MPR images. The incidence of the subarticular nerve (iSN) and the nerve root compression (iNRC) was respectively assessed on T2WI and axial 3D-FIESTA images. The shortest distance between the disc and the extraforaminal nerve root (DA) and between the foramen nerve root and the structures anterior to the facet joint capsule (DB) were measured in axial 3D-FIESTA images.Results
3D-FIESTA (100%, 100%) showed significantly higher iSN of L4/5 in all the subjects and iNRC in patients with LDH than T2WI (91.3%, 38.1%) (P<0.05)(Table 1). The DA of L4/5 and L5/S1 were significantly higher in healthy volunteers than that in patients with LDH (P<0.05)(Table 2). In healthy volunteers, the DA of L5/S1 was the smallest and that of L1/2 was the highest (P<0.05) and the DB of L4/5 was the smallest and that of L2/3 was the highest (P<0.05).Discussion
The ISN of L4/5 on 3D-FIESTA (100%) was significantly higher than that on T2WI (91.3%) in all the subjects (P<0.05). The iNRC on 3D-FIESTA (100%) was significantly higher than that on T2WI (38.1%) in patients with LDH (P<0.05). At the site of disc herniation on T2WI sequence, the nerve root is close to the disc so that the nerve root cannot be clearly shown due to the partial volume artifacts.4-5 In addition, layer thickness was the major factor in display of the actual contact between nerve root and disc on T2WI sequence. The 3D-FIESTA sequence with the feature of relatively thinner slices reduced partial volume artifacts and showed the nerve bundles more clearly due to contiguous thin slices and MPR. Therefore, the compressed nerve roots could be distinguished from normal ones and the detection rate of the actual contact between nerve root and disc could be elevated. There was no significant difference of DA and DB between the left and right sides. The DA of L4/5 and L5/S1 were significantly higher in healthy volunteers than that in patients with LDH (P<0.05). There are few studies about the compression of extraforaminal nerve root in patients with central/paracentral lumbar disc herniation. Our study showed that the distance between the disc and the extraforaminal nerve root in patients with LDH was smaller than that in healthy people, and most of the discs were in contact with nerve roots. Degenerative discs might cause mechanical compression of nerve roots. Patients with LDH were often accompanied with compression of extraforaminal nerve root caused by disc bulge. In healthy volunteers, less DA of L5/S1 over L1/2 while higher DB of L2/3 over L4/5 (P<0.05) showed normally altered morphometry. The diameter of lumbar nerve root gradually increased from L1 to L5.8 Most L4 dorsal root ganglion is located intraforaminally, while most L5 dorsal root ganglion is located extraforaminal.9 The results may further explain the high incidence of L4 and L5 radiculopathy, especially the thickening of posterior ligamentum flavum, hyperosteogeny and disc bulging taken into consideration.Conclusion
3D-FIESTA-C sequence can clearly show nerve root compression in patients with LDH. With the normal anatomical structures shown on 3D-FIESTA-C images, clinicians could more comprehensively and easily realize and seize the conditions of nerve root compression and further reduce the misdiagnosis rate.Acknowledgements
No acknowledgement found.References
1. Lou ZH, Qu JR, Li HL, et al. Optimal technique of three-di-mensional MRI of the lumbar nerve root and its radicular vein in normal and lumbar disc herniation patients [J]. Chin Med J,2011, 124(12): 1802-1806.
2. Kobayashi S, Takeno K, Yayama T, et al. Patho mechanisms ofsciatica in lumbar disc herniation: effect of periradicular adhesivetissue on electro physiological values by an intraoperative straight leg raising test [J]. Spine, 2010, 35(22): 2004-2014.
3. Hossein J, Fariborz F, Mehrnaz R, Babak R. Evaluation of diagnostic value and T2-weighted three-dimensional isotropic turbo spin-echo (3D-SPACE) image quality in comparison with T2-weighted two-dimensional turbo spin-echo (2D-TSE) sequences in lumbar spine MR imaging. Eur J Radiol Open. 2018;6:36-41.
4. J. Sung, W.-H. Jee, J.-Y. Jung, et al. Diagnosis ofnerve root compromise of the lumbar spine: evaluation of the performance of three-dimensional isotropic T2-weighted turbo spin-echo SPACE sequence at 3T, Korean J. Radiol. 18 (1) (2017) 249–259.
5. Lee S, Jee WH, Jung JY, et al. MRI of the lumbar spine: comparison of 3D isotropic turbo spin-echo SPACE sequence versus conventional 2D sequences at 3.0 T. Acta Radiol 2015;56:174-181
6. Jiang SD, Jiang LS, Dai LY, et al. Extreme lateral lumbar disc herniation in a 12-year child: case report and review of the literature[J]. Eur Spine J, 2010, 19(Suppl 2N): S197-S199.
7. Lewis AM, Layzer R, Engstrom JW, et al. Magnetic resonance neurography in extraspinal sciatica[J]. Arch Neurol, 2006, 63(10):1469-1472.
8. Hasegawa T, Mikawa Y, Watanabe R, An HS. Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine (Phila Pa 1976). 1996;21(9):1005-1009.
9. Leng L, Liu L, Si D. Morphological anatomy of thoracolumbar nerve roots and dorsal root ganglia. Eur J Orthop Surg Traumatol. 2018;28(2):171-176.
Figures