4529
Improved Visualization of MR Neurography in the Cervical Nerve Roots using Accelerated Quantitative Double Echo Steady-State (qDESS)
Yutaka Hamatani1, Kayoko Abe2, Yasuhiro Goto1, Masami Yoneyama3, Quin Lu4, Isao Shiina1, Kazuo Kodaira1, Takumi Ogawa1, Mana Kato1, Michinobu Nagao2, and Shuji Sakai2
1Department of Radiological Services, Tokyo Women's Medical University, Tokyo, Japan, 2Department of Diagnostic imaging & Nuclear Medicine, Tokyo Women's Medical University, Tokyo, Japan, 3Philips Japan, Tokyo, Japan, 4Philips Healthcare NA, San Francisco, CA, United States
1Department of Radiological Services, Tokyo Women's Medical University, Tokyo, Japan, 2Department of Diagnostic imaging & Nuclear Medicine, Tokyo Women's Medical University, Tokyo, Japan, 3Philips Japan, Tokyo, Japan, 4Philips Healthcare NA, San Francisco, CA, United States
Synopsis
Accelerated quantitative double echo steady state (qDESS), which is combined with Compressed SENSE is expected to improve visualization of the cervical nerve roots and brachial plexus. The purpose of this study was to optimize flip angle (FA) and spatial resolution (3D voxel size) of accelerated qDESS to visualize the small nerve roots and brachial plexus in the cervical spine. As a result, a combination of FA: 35 degree and voxel size: 0.8mm3 was the most appropriate parameters to demonstrate them while suppressing the background signals including the muscles, blood vessels, and cerebrospinal fluid.
Introduction
Assessment of cervical nerve roots is important as well as the brachial plexus MR Neurography when deciding surgical procedures in some cases, such as traumatic brachial plexus injuries and neonatal brachial plexus palsy.1,2 Since the cervical nerve roots are the complex anatomy, such small nerves cannot be visualized well by the conventional MRI.3 We have demonstrated that the combined use of SHINKEI MR neurography4 and phase-cycling balanced SSFP (and its complex subtraction images) has been useful to visualize both the brachial plexus and nerve roots within a feasible scan time.5 However, it is still challenging to clearly visualize both the brachial plexus and nerve roots in a short scan time without motion misregistration because separately acquired two imaging datasets are required, one single scan would therefore be desired. Double Echo Steady-State (DESS) with water-selective excitation is a useful sequence to depict small nerves such as intracranial nerves,6,7 it would also be promising for visualizing cervical nerve roots. DESS sequence chart is shown in table1. Furthermore, 3D quantitative DESS (qDESS) offers a rapid simultaneous 3D morphometry and T2 relaxometry.8-10 Recently, accelerated qDESS sequence combined with compressed sensing sensitivity encoding (Compressed SENSE) has been proposed for rapid 3D knee morphological and quantitative imaging11. In this study, we evaluated appropriate parameters of accelerated qDESS to improve demonstration of both the cervical nerve roots and the brachial plexus within a short scan time.Methods
Five healthy volunteers (4 males, 1 female, age 25-45 years old) were examined by 3.0T MRI (Ingenia, Philips Healthcare). Suitable flip angle (FA) and 3D voxel size of accelerated qDESS were evaluated as follows; 1. Assessment of optimized FA FA was set to 15, 25, and 35 degrees to assess image contrast between the cervical nerves and surrounding background. The other parameters were: TR/TE1/TE2=17/5.0/12.3ms, FOV=200x200x120 mm, slice thickness=1.2 mm, slice number=200, acquisition time=2:32. 2. Assessment of optimized 3D voxel size 3D voxel size was set to 0.8mm3, 1.0mm3, 1.2mm3 (iso-voxel size) to evaluate visualization of both the nerve root and the brachial plexus. The imaging parameters were shown in Table 1. These visual evaluations were performed by three radiologists and radiological technologists using a 5-point scale: 0, non-evaluative; 4, excellent quality.Results and Discussion
Results and Discussion FA has a very important role for generating contrast between the cervical nerve roots and surrounding tissues, such as the muscles, cerebrospinal fluid, and blood vessels. The visual evaluation scores of accelerated qDESS using FA: 35 degree was significantly higher than others (Figure 2) and the brachial plexus were most clearly demonstrated using it. Accelerated qDESS using 0.8mm3 isotropic acquisition showed the most detailed anatomy of the ventral roots (Figure 3). Figure 4 was the representative accelerated qDESS images with optimized parameters: FA: 35 degree and 0.8mm3 isotropic acquisition. It could provide detailed anatomical structures of cervical nerve roots with sufficient spatial resolution, image contrast, and signal to noise ratio. The optimized accelerated qDESS images clearly demonstrated the entire cervical nerve roots and it can provide quantitative information.Conclusion
Accelerated qDESS clearly visualized the whole brachial plexus including small nerve roots with a quantitative information. It could be a helpful sequence to contribute to the diagnosis of nerve root and peripheral nerve disorders such as radiculopathy.Acknowledgements
No acknowledgement found.References
References 1. Somashekar D, et al. High-resolution MRI evaluation of neonatal brachial plexus palsy: A promising alternative to traditional CT myelography. AJNR Am J Neuroradiol. 2014 Jun;35(6):1209-13. 2. Yoshikawa T, et al. Brachial plexus injury: clinical manifestations,conventional imaging findings, and the latest imaging techniques. Radiographics. 2006 Oct;26 Suppl 1:S133-43. 5 3 Qi wang et al. Diagnostic agreement between 3.0-T MRI sequences of nerve root and surgery in patients with cervical radiculopathy. Medicine (Baltimore). 2021 Jan 29; 100(4): e24207. 4. Yoneyama M, et al. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci. 2013;12:111-9. 5. Tadenuma H, et al, MR Myelo-Neurography: Improved Visualization of MR Neurography in the Brachial Plexus using a Combination of SHINKEI and Phase-Cycling balanced SSFP. Proc. ISMRM:2018.3185. 6. Qin Y, et al. 3D double-echo steady-state with water excitation MR imaging of the intraparotid facial nerve at 1.5T: a pilot study. AJNR Am J Neuroradiol. 2011 Aug;32(7):1167-72. doi: 10.3174/ajnr.A2480. 7. Fujii H, et al. Visualization of the Peripheral Branches of the Mandibular Division of the Trigeminal Nerve on 3D Double-Echo Steady-State with Water Excitation Sequence. AJNR Am J Neuroradiol. 2015 Jul;36(7):1333-7. doi: 10.3174/ajnr.A4288. 8. Chaudhari AS. et al. Combined 5‐minute double‐echo in steady‐state with separated echoes and 2‐minute proton‐density‐weighted 2D FSE sequence for comprehensive whole‐joint knee MRI assessment. J Magn Reson Imag. 2019;49(7): e183-e194. 9. Lu Q, et al. Knee T2 relaxometry using quantitative DESS: reproducibility across imaging vendors. Proc. ISMRM:2019.4473. 10. Sveinsson B, et al. A simple analytic method for estimating T2 in the knee from DESS. Magn Reson Imaging. 2016;38:63-70. 11. Lu Q, et al. Application of Compressed Sensing to Quantitative Double Echo steady state (qDESS) for Rapid T2 Relaxometry in Knees. Proc. ISMRM:2020.2733.Figures
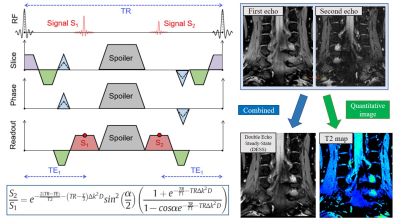
Figure 1.
Scheme of quantitative DESS imaging
DESS creates
two echoes with distinct contrast; the first echo has a high signal-to-noise
ratio (SNR) with contrast determined by the T1/T2 ratio, while the second echo
has greater T2-weighted contrast. A spoiler gradient is commonly included
between the two readouts to mitigate banding artifacts. T2 quantification was
performed by inverting the qDESS signal model.
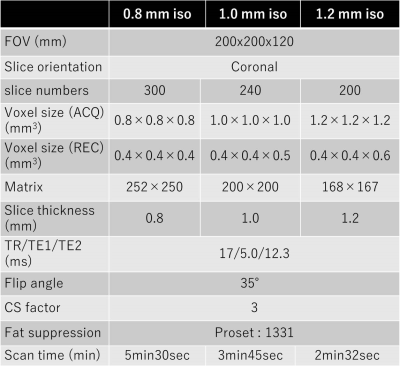
Table 1. Imaging parameters of accelerated qDESS for
optimization of voxel-size.
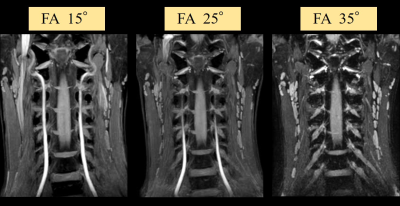
Figure 2. Comparison of accelerated qDESS with different flip angles for visualization of the cervical
nerves
Accelerated qDESS with FA: 35° shows the best contrast between surrounding
soft tissues and cervical nerves
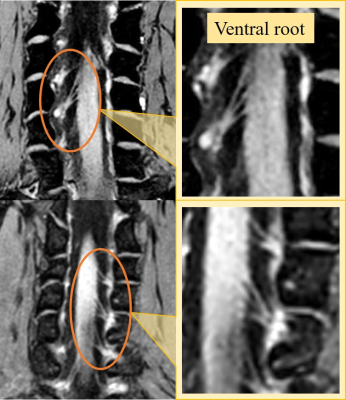
Figure 3.
Representative accelerated qDESS with
0.8mm isotropic images in the cervical nerve roots.
Accelerated qDESS with 0.8mm3 demonstrates the detailed anatomy of the
ventral roots.
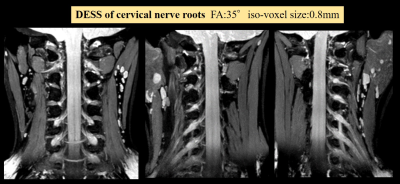
Figure 4. Representative accelerated qDESS images with optimized
parameters.
Accelerated qDESS with FA:35
degree and 0.8mm3 isotropic acquisition shows the detailed
anatomical structures of the cervical nerve roots with sufficient spatial
resolution, image contrast, and SNR.
DOI: https://doi.org/10.58530/2022/4529