4467
Detect the etiology of single small subcortical infarction with High Resolution-Vessel Wall Imaging1Department of Radiology, Tianjin Huanhu Hospital, Tianjin University, Tianjin, China, 2MR Collaboration, Siemens Healthineers Ltd., Beijing, China
Synopsis
This study used high resolution vessel wall imaging to investigate the lenticulostriate artery (LSA) morphology and plaque characteristics in three patient groups: single small subcortical infarction (SSI) with/without plaque on the parental artery, and large subcortical infarction with large artery atherosclerosis (LAA) as reference. SSI with plaque (SUD) on the parental artery manifested more like LAA, having relatively lower total CSVD score and lower number and total length of LSA branches. However, the plaques in SUD were mainly positive remodeling. These findings reinforce our understanding about the etiology of SSI with plaque on the parental artery.
Introduction and Purpose
The etiology of single subcortical infarction located in the blood supply area of the perforating artery remains controversial [1], mainly with two proposed vascular pathogeneses: 1) lipohyalinosis and fibrinoid of lenticulostriate artery (LSA) itself (termed SAD); 2) atherosclerosis in parental large artery that obstructs a proximal branch or orifice of LSA (termed LAA). Distinguishing between the two mechanisms is important for determining clinical treatment strategy. Clinically, the infarction size is used as main criterion for differentiation due to a lack of in-vivo imaging technique that can directly observe the plaque and orifice of LSA; Small subcortical infarctions (SSI) are classified as SAD type and large subcortical infarctions (LSI) are classified as LAA type. However, patients with SSI may also have LAA mechanism [1].High resolution vessel wall imaging (HR-VWI) is capable of imaging both large-vessel wall and the LSA lumen simultaneously [2]. We hypothesized that SSI with plaques and SSI without plaques may have different pathogenesis. This study aimed to investigate image indicators for diagnosing etiology of SSI using HR-VWI.
Method
Images from prospectively recruited patients with clinically confirmed isolated subcortical infarction from January 2017 to January 2021 were retrospectively analyzed. A total of 92 patients were enrolled, and all underwent routine MRI, time-of-flight MR angiography, and HR-VWI on a 3T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) with a 20-channel head-neck coil. HR-VWI was performed using the SPACE (Sampling Perfection with Application-optimized Contrast using different flip angle Evolutions) sequence with parameters: FOV=230×230 mm2, slices=240, voxel size=0.53×0.53×0.53 mm3, TR/TE=900ms/15ms, echo train length=52, scan time=8:07 mins.Based on routine MRI, the infarct information (infarct size, lowest layer position, and total number of layers) and total cerebral small vessel disease (CSVD) score were measured. The patients were divided into either LSI group or SSI group according to the size of lesion on diffusion weighted images. SSI was defined as: cross-sectional infarct with a maximum diameter <1.5cm and <3 cumulative slices. Based on South Korea's modified TOAST (Trial of Org 10172 in Acute Stroke Treatment, TOAST) classification, patients with plaques in the LSI group were classified as large artery atherosclerosis (LAA); patients with plaques in the SSI group were classified as the Stroke of undetermined etiology (SUD); while patients without plaques in the SSI group were classified as small vessel disease (SAD).
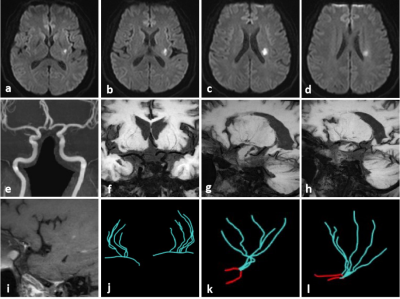
LSA morphology and plaque characteristics analysis for a representative patient from SUD group using HRVWI are shown in Figure 1. In post-processing of HRVWI, the LSA morphology was quantified by referring to a previous paper [2], which included number and laterality index (LI) for trunks, branches, and total length. LI is used to express the difference between the healthy side and the affected side. LAA, SUD, and SAD groups were further compared by using One-Way ANOVA or Kruskal-Wallis H test. Based on HRVWI, the arterial wall morphology and plaque characteristics such as wall area (WA), plaque area, plaque burden, remodeling index and pattern, and stenosis rate were quantified and compared between LAA and SUD group using two samples t-test or Mann-Whitey U test.
Results
The LSI group consisted of 45 patients; 30 patients (19 males) had detected atherosclerotic plaque in the M1 segment (LAA group). The SSI group consisted of 47 patients; 28 patients (22 males) had atherosclerotic plaque in the M1 segment (SUD group). The remaining 19 patients (16 males) had no plaque in the M1 segment (SAD group).The total CSVD score of LAA (P=0.001) and SUD groups (P=0.017) were significantly lower than SAD group.
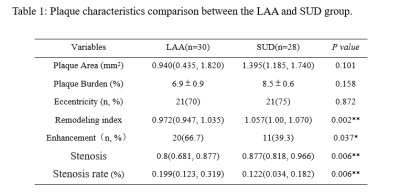
On the infarcted side, the number and total length of LSA branches in the LAA and SUD groups were shorter than those in the SAD group. Moreover, the total length LI of LSA in the LAA group and SUD group was greater than that in the SAD group. For plaque characteristics (Table 1), SUD group plaque enhancement ratio (P=0.037) and stenosis rate (P=0.006) were lower than those of the LAA group. SUD group remodeling index was significantly higher than that of the LAA group (P=0.002); positive remodeling was dominant in SUD (60.7%) while LAA was mainly non-positive remodeling (83.3%).
Discussion
The LAA group had lower total CVSD score, and the number and total length of LSA branches in LAA group were lower while the LI was larger. These findings are logical and support the atherosclerotic mechanism of LAA patients.The SAD group had higher total CVSD score, and the number and total length of LSA branches were longer while the LI was smaller. This also supports the mechanism of lipid hyalinization.
Similar to the LAA group, SUD group total CVSD score was relatively lower, and the number and total length of LSA branches were shorter while the LI was larger. However, different from LAA group, plaques in SUD were mainly positive remodeling.
Conclusion
In sum, SSI with plaques and SSI without plaques may have different pathogenesis. Those with plaques may have a coexisting mechanism of atherosclerosis, which manifests as a lower total CVSD score and a shorter total length of the LSA. Microemboli produced by unstable plaques may be a pathological mechanism of the occurrence of the small infarction.Acknowledgements
This project was supported by Tianjin Natural Science Foundation(20JCYBJC00960) and National Natural Science Foundation of China(2021B1-0203)References
[1] Rosner S S, Rhoton A J, Ono M, et al. Microsurgical anatomy of the anterior perforating arteries[J]. J Neurosurg, 1984,61(3):468-485.
[2] Zhang, et al. "Visualization of the lenticulostriate arteries at 3T using black-blood T1-weighted intracranial vessel wall imaging: comparison with 7T TOF-MRA." European Radiology. 2019;29: 1452-1459.
[3] Zhu T, Ren L, Zhang L, et al. Comparison of plaque characteristics of small and large subcortical infarctions in the middle cerebral artery territory using high-resolution magnetic resonance vessel wall imaging[J]. Quantitative Imaging in Medicine and Surgery, 2021,11(1):57-66.
Figures