4464
Multi-parametric imaging on cerebral infarction using MULTIPLEX1Radiology, Beijing Luhe Hospital, Capital Medical University, Beijing, China, 2UIH America, Inc., Houston, TX, United States, 3United Imaging Healthcare Co., Ltd., Shanghai, China
Synopsis
A state-of-the-art multi-parametric imaging method, namely MULTIPLEX, was evaluated for its potential for cerebral infarction. The MULTIPLEX method offered single-scan multi-contrast information with 3D high resolution images, not only showing the capacity to supplement or replace routine protocols for anatomical and edema imaging, but also offered additional information on bleedings and penumbra, showing the potential as an one-click solution for daily cerebral infarction imaging.
Introduction
Cerebral infarction (CI) is one of the worldwide leading causes of disability and death. An accurate measure of the severity of ischemic insult and the resulting prognosis is needed for personalized diagnosis and treatment evaluation. Routine MRI scanning protocols for CI generally consist of individual scans of T1W or T1-FLAIR, T2W or T2-FLAIR and diffusion weighted imaging (DWI) and susceptibility weighted imaging (SWI)1, all except SWI are based on 2D spin echo (SE) acquisitions. These scans have been widely proven and accepted clinically, yet still have their own short planks. The major issue of 2D imaging methods lies in their thick slices with spatial gaps, which lead to strong partial volume effects and/or failure to capture small lesions located at the gaps. Second, different scans may have different spatial settings, and patient motion between scans may lead to lesion mismatch. Thirdly, total scan times of a complete CI protocol set, including the 3D SWI, can be too long for CI patients.In this work, we conducted an initial test of a newly developed single-scan multi-parametric imaging method, i.e. MULTIPLEX2, on a CI patient to evaluate its potential to reveal pathological and anatomical information.
Methods
With local IRB approval, one CI patient (male, 65/yro) with subacute stroke in the corona radiata region was recruited and scanned with CT and MRI 4 days after onset. CT results (not shown) reported no cerebral hemorrhage.All MRI scans were performed on a 3T system (uMR780, United Imaging Healthcare, Shanghai ,China) with a 24-channel head coil. Routine scans included: 1) axial T1-FLAIR (TI=870ms, TE/TR=10/2010ms, 2x interpolated in-plane resolution 0.45x0.45mm2, TA=1’29” with 2.3x compress sensing (CS)); 2) axial T2-FLAIR (TI=870ms, TE/TR=10/2010ms, 2x interpolated in-plane resolution 0.5x0.5mm2, TA=1’20” with 2.3x CS); 3) an axial T2-FSE (TE/TR=96/4000ms, 2x interpolated in-plane resolution 0.38x0.38mm2, TA=40” with 2.2x CS); and 4) axial EPI-DWI (b = 0&1000s/m, TE/TR=78/4000ms, 2x interpolated in-plane resolution 0.72x0.72mm2, TA=60” with 2x parallel imaging). All routine scans generated 20 slices with 5mm thickness and 1.5mm gap, and combined scan time of 4’29”.
For MULTIPLEX scan, the scanning protocol was: FA1/FA2=4°/16°, TR1/TR2=8.2/27.9ms, 5x echoes with TE=3.76~23.36ms, bandwidth=230Hz/px, in-plane resolution (not interpolated) 0.70x0.70mm2, slice thickness=1.5mm (interpolated from 3mm), and TA=3’19” with 4x parallel imaging using wave readouts3. Virtual FLAIR (vFLAIR) images were generated via the MULTIPLEX tier-3 post processing2 using proton density-weighted (PDW) images and T1 map.
Results
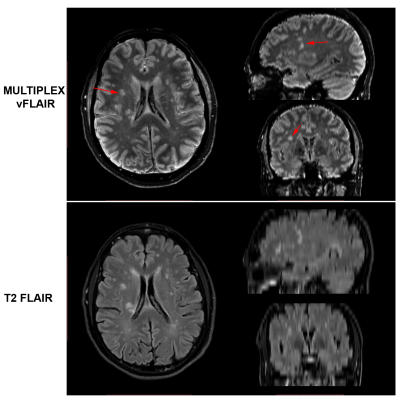
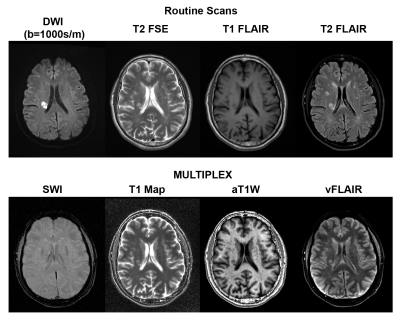
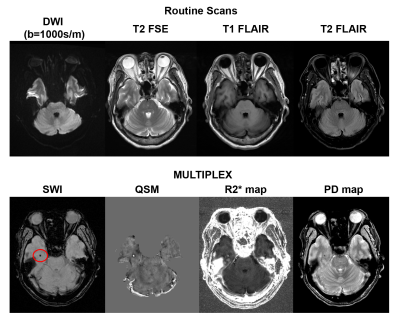
Figure 1 compares the MULTIPLEX vFLAIR images to the routine T2-FLAIR images on the capacity of revealing hyperintense infarct lesions in 3D views. Figure 2 compares the images between routine images (DWI/T2-FSE/T1- and T2-FLAIR) and MULTIPLEX images on a typical slice, showing similarities in image contrast information between MULTIPLEX images vs. routine scans of T2-FSE, T1-FLAIR and T2-FLAIR. Figure 3 shows another slice of images, where a cerebral microbleed (CMB) located in right temporal white matter was clear seen in MULTIPLEX images but was obscured in all routine scans.Discussion
In this study, we have for the first time evaluated the potential of the MULTIPLEX2 method for CI imaging, suggesting MULTIPLEX not only can offer similar information as with routine T2-FSE, T1- and T2-FLAIR scans, but also offers additional capacity for CMB detection.T2-FLAIR is basically the gold standard for detecting hyperintense infarct lesions4. However, due to the long scan time in 3D mode5, T2-FLAIR generally produce 2D slices that are thick (for sufficient SNR) and with gaps (to avoid RF crosstalk),for small lesions this not only may lead to reduced detectability due to partial volume effects, but also have the risk of non-detection for those physically located between slice gaps. Therefore some CI protocols would include a second or even a third T2-FLAIR scan with orthogonal planes to ensure the capture of all lesions, at the cost of prolonged scan time. On the other hand, PDW images have also been demonstrated6 to reliably detect white matter lesions, and by combining the PDW contrast and CSF suppression effect via virtual inversion recovery, the resultant MULTIPLEX vFLAIR images was able to detect all lesions with better delineation in high resolution 3D views (Fig.1). However, it should be noted that the lesion contrast in MULTIPLEX vFLAIR was not as salient as T2-FLAIR, making some of the lesions not easy for detection unless using T2-FLAIR as reference. Therefore, MULTIPLEX vFLAIR can be used as supplementary information to T2-FLAIR.
The MULTIPLEX’s T1 map and aT1W offered highly similar anatomical contrast with routine T2-FSE and T1-FLAIR (Fig.2), suggesting the possibility of substitution for these two scans. However, DWI remained the most sensitive and only method to detect the ischemic infarct core (Fig.2), the combination of its lack of SWI contrast suggested acute/sub-acute stage. With susceptibility sensitivity, several MULTIPLEX images detected a CMB in the right temporal lobe (Fig.3), which was not shown in any routine images nor the patient’s CT scan. The functionality of SWI can be fully realized with MULTIPLEX. And with state-of-the-art acceleration techniques3, the additional cost on scan time can be minimal.
Conclusion
In conclusion, we have demonstrated the potential of MULTIPLEX method for CI imaging, which may have the potential as the supplementary or replacement to some of the routine scans.Acknowledgements
No acknowledgement found.References
1. https://radiopaedia.org/articles/stroke-protocol-mri?lang=us
2. Ye Y, Lyu J, Hu Y, Zhang Z, Xu J, Zhang W. MULTI-parametric MR imaging with fLEXible design (MULTIPLEX). Magn Reson Med 2021.
3. Qiu Z, Jia S, Su S, et al. Highly accelerated parallel MRI using wave encoding and virtual conjugate coils. Magn Reson Med 2021;86(3):1345-1359.
4. Brant-Zawadzki M, Atkinson D, Detrick M, Bradley WG, Scidmore G. Fluid-attenuated inversion recovery (FLAIR) for assessment of cerebral infarction. Initial clinical experience in 50 patients. Stroke 1996;27(7):1187-1191.
5. Naganawa S, Koshikawa T, Nakamura T, et al. Comparison of flow artifacts between 2D-FLAIR and 3D-FLAIR sequences at 3 T. European radiology 2004;14(10):1901-1908.
6. Schmidt C, Hattingen E, Faehndrich J, Jurcoane A, Porto L. Detectability of multiple sclerosis lesions with 3T MRI: a comparison of proton density-weighted and FLAIR sequences. J Neuroradiol 2012;39(1):51-56.
Figures