4463
Association and Prediction of Intracranial Plaque Characteristics and Hs-CRP Levels In Patients with Acute Cerebral Infarction1Jiangsu Key Laboratory of Molecular and Functional Imaging, Department of Radiology, Zhongda Hospital, Medical School, Southeast University, Nanjing, China, 2Philips Healthcare, Shanghai, China
Synopsis
Atherosclerosis accompanied by inflammation is considered to be a crucial mechanism for patients with ischemic stroke. We aimed to investigate the association between intracranial plaque characteristics and high-sensitivity C-reactive protein (hs-CRP) levels to predict the occurrence of acute cerebral infarction (ACI). 85 patients with cerebral infarction were divided into ACI group and non-acute cerebral infarction (NACI) group. Hs-CRP levels were further grouped into low, intermediate and high groups. We concluded that elevated hs-CRP levels was independently associated with strong plaque enhancement, their synergistic effects provided incremental value in predicting the occurrence of acute cerebral infarction.
INTRODUCTION
Ischemic stroke is a major cause of death and disability worldwide. Intracranial atherosclerosis (ICAS) performs a vital role in Chinese patients with ischemic stroke, accounting for approximately 30~50% of the causes of stroke in Asian population 1,2. Inflammation is considered to be a crucial mechanism for the progression of atherosclerosis. Serum levels of high-sensitivity C-reactive protein (hs-CRP) have been identified as a new target for monitoring atherosclerosis and cerebrovascular events. However, perhaps due to the limitations of intracranial plaque imaging technology, the relationship between intracranial plaque characteristics and hs-CRP levels in patients with ischemic stroke is unclear. We aimed to investigate the association between hs-CRP levels and intracranial plaque characteristics displayed on high-resolution magnetic resonance (HR-MRI) vascular wall imaging, and their combined predictive contribution to the occurrence of acute cerebral infarction.METHODS
85 patients with cerebral infarction in the territory of the middle cerebral artery (MCA) or basilar artery (BA) were enrolled and divided into acute cerebral infarction (ACI) group (n=61) and non-acute cerebral infarction (NACI) group (n=24) according to clinical data and DWI images. All recruited patients underwent HR-MRI vascular wall imaging on a 3.0T MRI scanner to assess intracranial atherosclerotic plaque. Hs-CRP levels were measured and further grouped into: low group (hs-CRP<1 mg/L), intermediate group (1mg/L≤hs-CRP<3mg/L), and high group (hs-CRP≥3 mg/L), with the low group as the reference group for ACI predication. Plaque characteristics include plaque enhancement, standardized wall index (NWI), stenosis ratio, T1 hyperintense component, remodeling pattern, plaque area (PA), plaque burden (PB) and maximum wall thickness (Max WT). Plaque features, demographic and clinical characteristics were compared between ACI group and NACI group. The correlation between intracranial plaque characteristics and hs-CRP levels was calculated with Spearman correlation analysis. Multivariate logistic regression and receiver operating characteristic (ROC) curves were constructed to determine the association between plaque features and hs-CRP levels as well as their combined effects on the occurrence of ACI.RESULTS
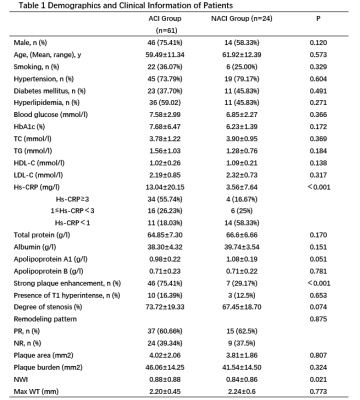
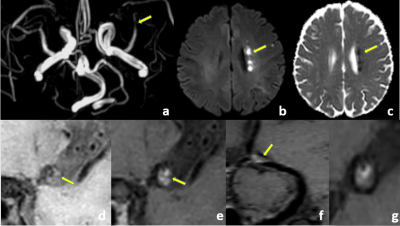
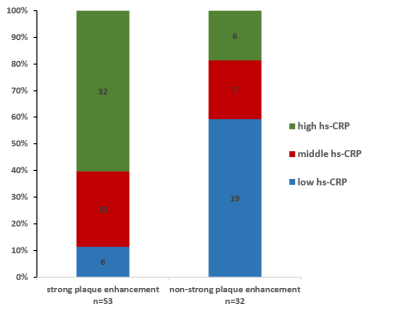
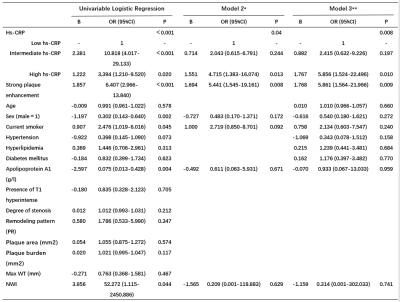
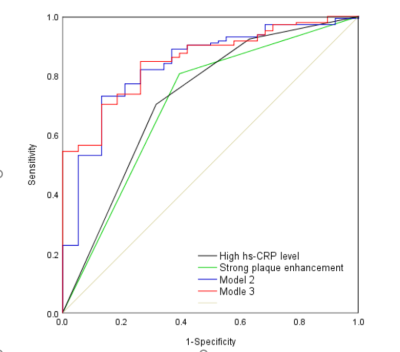
Table 1 summarized the demographics and plaque characteristics of the ACI group and NACI group, the hs-CRP levels were 13.04 ± 20.15 mg/L and 3.56 ± 7.64 mg/L (p<0.001), respectively. More plaques in ACI group showed strong enhancement compared to that of NACI group (p<0.001) (Table 1, Figure 1). Strong plaque enhancement was positively correlated with hs-CRP (r=0.504, p<0.001). The distribution of strong plaque enhancement in relation to hs-CRP levels was illustrated in Figure 2. In multivariate logistic regression, elevated hs-CRP levels were associated with strong plaque enhancement independently of age and other plaque features (Model 1) (p < 0.001, odds ratio [OR] 7.860, 95% confidence interval [CI] 3.538~17.463). Strong plaque enhancement (p<0.009,OR 5.861,95% CI 1.564~21.966) and high hs-CRP level (p<0.01,OR 5.856,95% CI 1.524~22.496) were found to be independent high-risk factors for the prediction of ACI before (Model 2) and after adjustment of age and other atherosclerotic risk factors (Model 3) (Table 2). The combination of hs-CRP levels and strong plaque enhancement provided incremental information with an area under the receiver operating characteristic curve (AUC) (95% confidence interval) of 0.854 (0.795~0.912), which was significantly higher than that of strong plaque enhancement (AUC 0.706(0.607~0.806)) and high hs-CRP level (AUC 0.723 (0.624~0.821)), respectively (Figure 3).DISCUSSION
A positive relationship between gradually increasing hs-CRP levels and strong plaque enhancement was observed in our study, and elevated hs-CRP levels were independently associated with stronger plaque enhancement. Intracranial plaque enhancement has been recognized as a marker of inflammation and plaque instability 3,4. It has been proven that strongly enhanced plaque had more severe inflammation response that could accelerate the progression of atherosclerotic plaque instability 5. Our findings supported that inflammation indicators hs-CRP might be a significantly useful predictor in the presence of intracranial strongly enhanced plaque, which might impact the development of atherosclerosis plaque through its involvement in complex pathways of mediating immune inflammatory response 6.7. We also found that high hs-CRP level and stronger plaque enhancement were potential risk factors for ACI, the combination of them provided higher predictive value to identify the occurrence of ACI as compared to their individual predictive ability, especially for patients with hs-CRP≥3 mg/L. It is postulated that high level of hs-CRP may mediate the inflammatory response and endothelial dysfunction to accelerate the cumulative damage and shedding of unstable atherosclerotic plaques, further increasing the likelihood of significant stenosis of cerebrovascular vessels, which ultimately led to the occurrence of ipsilateral ACI and extensive tissue damage 8. Our findings extend this association from carotid artery atherosclerosis to ICAS 9, further strengthening the evidence that the inflammatory effect of high hs-CRP level and the instability of strongly enhanced plaque can together improve the prediction ability of ACI. As an easily obtainable inflammatory index, hs-CRP may play an important role in the atherosclerosis process in ACI patients with strongly enhanced plaques.CONCLUSION
Elevated hs-CRP levels appear to be associated with strong plaque enhancement. The synergistic effects of high hs-CRP level and strong plaque enhancement have the potential to provide incremental value in identifying the occurrence of acute cerebral infarction.Acknowledgements
This study was supported by the Natural Science Foundation of Jiangsu Province of China(BK20170704), the Science Fund for Creative Research Groups of the National Natural Science Foundation of China(61821002) and the program of Jiangsu Provincial Commission of health and family planning of China (M2020041).References
1. Feldmann E, Daneault N, Kwan E, Ho KJ, Pessin MS, Langenberg P, et al. Chinese-White Differences In the Distribution Of Occlusive Cerebrovascular-Disease. Neurology. 1990;40(10):1541-5.
2. Bos D, Portegies MLP, van der Lugt A, Bos MJ, Koudstaal PJ, Hofman A, et al. Intracranial Carotid Artery Atherosclerosis and the Risk of Stroke in Whites The Rotterdam Study. Jama Neurol. 2014;71(4):405-11.
3. Qiao Y, Zeiler SR, Mirbagheri S, Leigh R, Urrutia V, Wityk R, et al. Intracranial plaque enhancement in patients with cerebrovascular events on high-spatial-resolution MR images. Radiology. 2014;271(2):534-42.
4.Skarpathiotakis M, Mandell DM, Swartz RH, Tomlinson G, Mikulis DJ. Intracranial Atherosclerotic Plaque Enhancement in Patients with Ischemic Stroke. Am J Neuroradiol. 2013;34(2):299-304.
5.Puz P, Lasek-Bal A, Ziaja D, Kazibutowska Z, Ziaja K. Inflammatory markers in patients with internal carotid artery stenosis. Arch Med Sci. 2013;9(2):254-60.
6. Pepys MB, Hirschfield GM, Tennent GA, Gallimore JR, Kahan MC, Bellotti V, et al. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature. 2006;440(7088):1217-21.
7. Lagrand WK, Niessen HWM, Wolbink GJ, Jaspars LH, Visser CA, Verheugt FWA, et al. C-reactive protein colocalizes with complement in human hearts during acute myocardial infarction. Circulation. 1997;95(1):97-103.
8. Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Frontiers In Immunology. 2018;9.
9.Eltoft A, Arntzen KA, Wilsgaard T, Hansen JB, Mathiesen EB, Johnsen SH. Joint Effect of Carotid Plaque and C-Reactive Protein on First-Ever Ischemic Stroke and Myocardial Infarction? J Am Heart Assoc. 2018;7(11).
Figures