4446
Cardiac and Respiratory-Resolved Image Reconstruction with the Beat Pilot Tone1Electrical Engineering and Computer Sciences, University of California, Berkeley, Berkeley, CA, United States
Synopsis
We have previously proposed Beat Pilot Tone (BPT), a motion sensing method using ultra-high-frequency RF and preamplifier intermodulation. BPT uses ultra-high-frequencies, which provides greater sensitivity to motion compared to the Pilot Tone (PT). In this work, we use the motion estimates from the BPT to reconstruct respiratory and cardiac-resolved images and compare them to motion-resolved images obtained using PT, respiratory bellows, and electrocardiogram (ECG) data. We show that BPT provides comparable image quality to conventional motion sensing for respiratory and cardiac motion.
Introduction
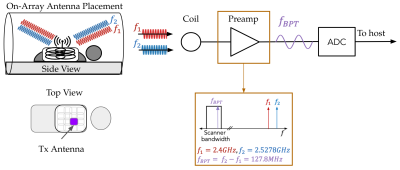
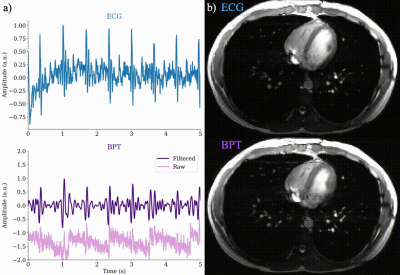
Accurate motion sensing in MRI is essential to correct for physiological motion that inevitably arises during the acquisition. Conventional motion sensing requires a suite of sensors or sequence-specific changes (e.g. navigators) and may be inconsistent between subjects.The Pilot Tone (PT) navigator has been established as a promising alternative1-4. PTs are pure tones within the MR bandwidth that are modulated by patient motion and received by the receiver coils. The PT contains respiratory and cardiac information which can be easily processed from the acquired data1-4; however, the PT frequency is tied to the Larmor frequency and may have limited sensitivity to motion within the body5. Previously, we proposed the Beat Pilot Tone (BPT) method, which improves upon this limitation by transmitting two ultra-high-frequency (UHF) tones separated by the desired BPT frequency within the bandwidth of the MR receiver. These tones are mixed in the preamplification stage via intermodulation to create a beat frequency that is digitized by the receiver chain, as shown in Figure 1.We have previously demonstrated that the BPT provides motion estimates that have greater sensitivity than the PT5. We now aim to show that motion estimates from the BPT yield improved image quality. In this work, we used three sources of motion sensing: the BPT, PT, and a conventional sensor (bellows for respiratory motion and electrocardiogram (ECG) for cardiac motion). The BPT produces comparable respiratory-resolved images to those binned by the PT and bellows. Additionally, the BPT produces cardiac-resolved images similar to the images corrected using ECG.
Methods
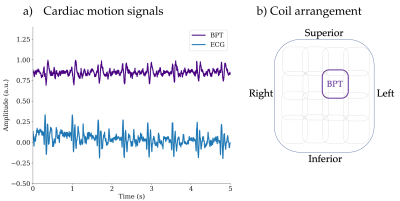
AcquisitionThe Beat Pilot Tone motion correction method was validated with in-vivo data on a GE 3T MR750W System. Three scans were acquired on a healthy volunteer: a free-breathing abdominal scan using a balanced SSFP imaging sequence and a 32-channel combined anterior and posterior array coil (FIESTA, TR=5.8 ms, FA=35, resolution=1.4mm), a breath-held cardiac scan with imaging gradients off (TR=3.5ms) to reduce noise in the BPT, and a breath-held cardiac scan (FIESTA, TR=4.6ms, FA=35, resolution=1.8mm) with the same array coil and imaging gradients on. The BPT and the PT were transmitted simultaneously and equalized to similar received levels using the hardware setup shown in Figure 1. Each BPT frequency was controlled by an Ettus Research B200 software-defined radio (SDR; National Instruments, TX, USA), synchronized to the system 10MHz clock. The PT was transmitted using a waveform generator (Siglent SDG6022X, Siglent Technologies, OH, USA). The chosen BPT frequencies were 2.4GHz and 2.5278GHz. The chosen PT frequency was 127.6MHz. A panel antenna placed on the chest was used for transmitting the PT and BPT (Figure 1). Floating cable traps6 were placed on the cable connected to the antenna to attenuate common-mode currents induced on the shield of the cable due to the transmit RF. For conventional motion sensing, respiratory bellows and ECG data were collected simultaneously. The motion-modulated BPT and PT signals were then extracted from each coil using the methods described previously1-5.
For the respiratory scan, the BPT and PT motion signals were selected from the coil with the most energy in the respiratory frequencies then low-pass filtered with a cutoff of 0.5Hz. For the second cardiac scan, the BPT was extracted from an anterior coil above the heart and band-pass filtered between 5 and 15Hz.
Reconstruction
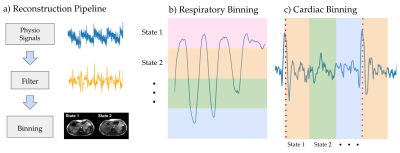
The raw MR data was binned into motion states using the filtered motion signal with respiratory binning (Figure 2b) and cardiac binning (Figure 2c). The free-breathing abdominal data was binned into six respiratory motion states, and the breath-held cardiac data was binned into five cardiac phases. The data in each motion state was averaged and coil-combined using the root sum of squares.
Results
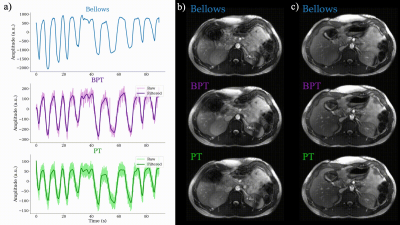
The results for the respiratory experiment are shown in Figure 3. Figure 3a shows the respiratory motion estimates from BPT, PT, and the bellows, respectively. Figure 3b shows the corresponding corrected images. All images have similar quality; however, images corrected using BPT and PT have some respiratory motion artifacts. Figure 4 shows the results of the first cardiac scan, a comparison between BPT with gradients off and ECG. The ECG is resampled to the BPT time resolution (3.5ms). Figure 4 suggests that the ECG and BPT provide comparable cardiac motion estimates, since the peaks are well aligned in time. Figure 5 shows the estimated cardiac signals from BPT and ECG (Figure 5a) and the reconstructed cardiac images (Figure 5b). The images have comparable quality; however, the BPT-reconstructed images show slight residual motion artifacts.Conclusion
We have shown that the BPT method is able to resolve respiratory and cardiac motion with comparable image quality to conventional motion sensing. The BPT, PT, and bellows produced similar respiratory-resolved images. The BPT provides similar cardiac information compared to ECG, and also produces cardiac-resolved images with similar quality, though some motion artifacts are visible.Acknowledgements
We sincerely thank Shreya Ramachandran for providing insight on binning and image reconstruction techniques and Karthik Gopalan for his help with designing and constructing the floating cable traps.References
1. Falcão, M. B., Di Sopra, L., Ma, L., Bacher, M., Yerly, J., Speier, P., ... & Roy, C. W. (2021). Pilot tone navigation for respiratory and cardiac motion‐resolved free‐running 5D flow MRI. Magnetic resonance in medicine.
2. Vahle, T., Bacher, M., Rigie, D., Fenchel, M., Speier, P., Bollenbeck, J., ... & Boada, F. E. (2020). Respiratory Motion Detection and Correction for MR Using the Pilot Tone: Applications for MR and Simultaneous PET/MR Exams. Investigative radiology, 55(3), 153.
3. Ludwig J, Speier P, Seifert F, Schaeffter T, Kolbitsch C. Pilot tone-based motion correction for prospective respiratory compensated cardiac cine MRI. Magn Reson Med. 2021.
4. Solomon E, Rigie DS, Vahle T, Paska J, Bollenbeck J, Sodickson DK, et al. Free-breathing radial imaging using a pilot-tone radiofrequency transmitter for detection of respiratory motion. Magn Reson Med. 2021.
5. Anand S, Lustig M. Beat Pilot Tone: Exploiting Preamplifier Intermodulation of UHF/SHF RF for Improved Motion Sensitivity over Pilot Tone Navigators. ISMRM Meeting and Exhibition Abstract. 2021.
6. Seeber, D. A., Jevtic, J., & Menon, A. (2004). Floating shield current suppression trap. Concepts in Magnetic Resonance Part B: Magnetic Resonance Engineering: An Educational Journal, 21(1), 26-31.
Figures