4437
CMR of fetal cardiac function and blood flow with doppler ultrasound cardiac gating
Erin K Englund1, Lorna P Browne1, Takashi Fujiwara1, Richard Friesen2, Mehdi H Moghari1, and Alex J Barker1
1Radiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States, 2Pediatric Cardiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
1Radiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States, 2Pediatric Cardiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
Synopsis
Fetal CMR is difficult due to the lack of an ECG signal, fetal motion, small anatomic sizes and high fetal heart rates. Initial results are presented which use a doppler ultrasound gating device to capture fetal cardiac motion in standard cardiac views and blood flow was quantified with 4D flow MRI. bSSFP cine images were scored for image quality by two radiologists and flow in the umbilical vein, ascending aorta and main pulmonary artery were quantified and agreed well with reported values. Unique insight was provided with dynamic imaging regarding the fetal circulation and the impact of congenital disease.
Introduction
High resolution imaging of fetal cardiac function and flow by MRI remains difficult due to fetal motion, small anatomic sizes, and high fetal heart rates (>130bpm). The use of doppler ultrasound-gating (DUS) for cine and 4D flow [1] MRI hold promise for overcoming these challenges. In particular, the fetal cardiovascular system has several distinctive features that are difficult to visualize or quantify, including blood flow in the umbilical vein, ductus venosus, ductus arteriosus, and foramen ovale. Additionally, it is imperative that normal anatomic variance is understood to detect abnormalities in the setting of congenital disease. The purpose of this abstract is therefore to demonstrate our experience using DUS-gated cine MRI to capture fetal cardiac motion and the preliminary utility of 4D flow MRI to visualize and quantify the unique features of the fetal circulation in volunteers and patients.Methods
In this IRB-approved study with ongoing recruitment, ten healthy pregnant volunteers (gestational age = 34.6±1.4 weeks) were scanned at 1.5T (n=6) or 3T (n=4) (Philips Ingenia MRI). Two patients, one with congenital diaphragmatic hernia (CDH, GA=35 weeks), and one with craniosynostosis (GA=30 weeks) were scanned at 1.5T. Images were obtained using a torso coil with the volunteers lying supine/decubitus according to comfort. Scout images were acquired to determine the location of the fetal heart. Once verified, a DUS gating device (Northh Medical) [2,3] was positioned superficially over the fetal heart and secured tightly with an elastic band. Localizers were repeated to ensure proper placement of the doppler probe and to plan fetal cardiac acquisitions. Cine balanced steady-state free precession (bSSFP) images of the fetal heart were acquired in the axial plane. If possible (dictated by amount of fetal motion) a combination of images were also acquired in standard cardiac planes (Figure 1). When achievable, anatomical images were acquired during maternal breath-hold. Following cine acquisitions, and provided that a consistent fetal cardiac gating signal persisted, 4D flow data were acquired. Pulse sequence parameters are summarized in Figure 2. Flow in the umbilical vein, ascending aorta, and main pulmonary artery were quantified using EnSight (Ansys, Inc.). Two radiologists scored short-axis (SA) bSSFP cines for sharpness, SNR, and lack of artifact on a 5-point Likert scale (5:excellent, 4:good, 3:satisfactory, 2:marginal 1:unusable).Results
Fetal CMR was not achieved in one volunteer due to lack of a reliable gating signal. In an additional 3 volunteers, fetal motion and/or time prevented the ability to acquire 4D flow data. Therefore, cine bSSFP images of the fetal heart were obtained in 9 volunteers, with 4D flow data in 6. Two of the volunteer 4D flow datasets were not of sufficient quality for quantitative analysis (due to fetal motion or ineffective gating). Across all 9 healthy volunteers, the average fetal heart rate was 139±7 bpm. Example short-axis views acquired at 1.5T and 3T are shown in Figure 1. Likert scoring for image quality was not different for the SA views at 1.5T and 3T (average scores of 4.2±0.8 and 4.2±0.8, respectively). Figure 3 and 4 show a 4D flow pathline visualization of the fetal circulation in a healthy volunteer. Across the four volunteer subjects, average flow in the ascending aorta was 1.5±0.7 mL/beat, main pulmonary artery was 2.3±0.7 mL/beat, and umbilical vein was 1.5±1.0 mL/beat. In the two patients, a limit of 15 minutes for research ‘add-ons’ prevented the acquisition of 4D flow data; however, both patients had diagnostic quality cine bSSFP images. Example fetal CMR images for the CDH patient are shown in Figure 5 showing the stomach and liver compressing the left atrium and an underdeveloped left ventricle.Discussion
Use of DUS gating allowed acquisition of both cine images of the fetal heart as well as 4D flow MR data. Success rates and gating signal stability increased in later volunteers due to experience, careful doppler probe placement, and training of staff. A transition to 3T imaging in later volunteers allowed for fewer averages to be collected with equivalent SNR and image quality to 1.5T (see Figure 1 and Likert scores), resulting in faster imaging and less fetal motion artifact. Unique features of the fetal circulation, including blood flow in the umbilical vein and ductus venosus, shunting through the foramen ovale from the right to left atrium, and flow through the ductus arteriosus are visualized with 4D flow (Figure 3 and 4). These features are difficult to observe with other methods and the blood flow measurements were in agreement with prior reports (assuming a fetal weight of 1.5-2kg) [4, 5]. Diagnostic quality images were obtained in the patients, and, in the case of the CDH patient (Figure 5), the imaging of dynamic motion provided unique insight regarding potential causes of the underdeveloped left ventricle.Conclusion
The ability to use ‘off-the-shelf’ product sequences without the need for offline reconstruction is promising for DUS-based fetal cardiac gating to be adapted in clinical workflows, with the caveat that training is critical to avoid gating-signal dropout and fetal motion artifacts. Continued development of fast and motion-robust acquisitions will enhance our ability to reliably capture fetal cardiac motion and blood flow.Acknowledgements
No acknowledgement found.References
- Dyverfeldt P, Bissell M, Barker AJ, Bolger AF, Carlhall CJ, Ebbers T, Francios CJ, Frydrychowicz A, Geiger J, Giese D, Hope MD, Kilner PJ, Kozerke S, Myerson S, Neubauer S, Wieben O, Markl M. 4D flow cardiovascular magnetic resonance consensus statement. J Cardiovasc Magn Reson. 2015;17:72.
- Kording F, Yamamura J, de Sousa MT, Ruprecht C, Hedström E, Aletras AH, Ellen Grant P, Powell AJ, Fehrs K, Adam G, Kooijman H, Schoennagel BP. Dynamic fetal cardiovascular magnetic resonance imaging using Doppler ultrasound gating. J Cardiovasc Magn Reson. 2018; 20:17.
- Kording F, Schoennagel BP, de Sousa MT, Fehrs K, Adam G, Yamamura J, Ruprecht C. Evaluation of a Portable Doppler Ultrasound Gating Device for Fetal Cardiac MR Imaging: Initial Results at 1.5T and 3T. Magn Reson Med Sci. 2018;17:308-317.
- Prsa M, Sun L, van Amerom J, Yoo SJ, Grosse-Wortmann L, Jaeggi E, Macgowan C, Seed M. Reference ranges of blood flow in the major vessels of the normal human fetal circulation at term by phase-contrast magnetic resonance imaging. Circ Cardiovasc Imaging. 2014;7:663–70.
- Schrauben EM, Saini BS, Darby JRT, Soo JY, Lock MC, Stirrat E, Stortz G, Sled JG, Morrison JL, Seed M, Macgowan CK. Fetal hemodynamics and cardiac streaming assessed by 4D flow cardiovascular magnetic resonance in fetal sheep. J Cardiovasc Magn Reson. 2019;21:8.
Figures
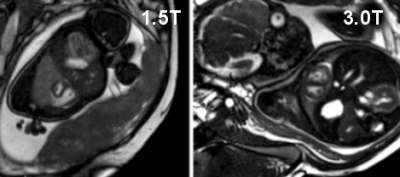
Short axis views acquired at 1.5T (gestational age, GA=32 weeks) and 3T (GA=35 weeks) during maternal breath-hold. The right and left ventricles are well visualized throughout the fetal cardiac cycle.
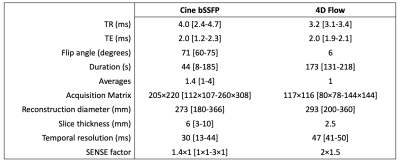
Summary of pulse sequence parameters for cine bSSFP and 4D flow acquisitions. Data are shown as mean [range] unless only one parameter value was used for all scans.
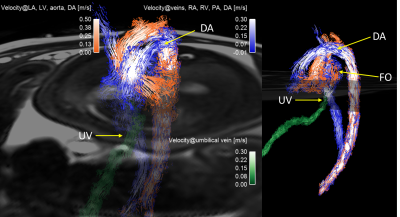
4D flow pathline
visualization in a volunteer (GA=35 weeks) in coronal and sagittal views,
showing flow in the umbilical vein/ductus venosus (UV, green), venous/right
heart (blue) and arterial/left heart (orange). Right and left heart pathlines
mix in the atria through the foramen ovale (FO) and in the descending aorta
post ductus arteriosus (DA).
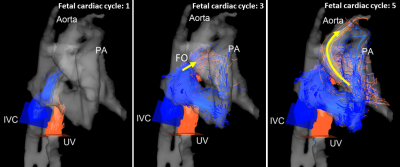
Unique
insight regarding the fetal circulation is visualized with 4D flow at 3T
(gestational age 35 weeks). Flow connectivity mapping follows the propagation of
umbilical vein/ductus venosus (UV, orange) and inferior vena cava (blue) blood
over the cardiac cycle. UV blood is found to traverse the foramen ovale (FO,
yellow arrow, cycle 3) and propagate into the aorta (yellow arrow, cycle 5).
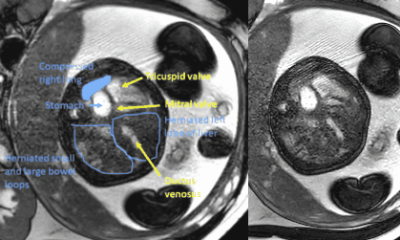
Fetal
CMR Cine bSSFP images at 1.5T of a congenital diaphragmatic hernia patient (35
weeks gestational age). The stomach and liver are seen compressing the left
atrium. The left ventricle is underdeveloped, and the right ventricle is
enlarged.
DOI: https://doi.org/10.58530/2022/4437