4379
Evaluation of Cerebral Blood Flow and BBB Water Exchange in an Aged African American Cohort1Laboratory of FMRI Technology (LOFT) Mark & Mary Stevens Neuroimaging and Informatics Institute Keck School of Medicine University of Southern California (USC), Los Angeles, CA, United States, 2Department of Ophthalmology and Department of Preventive Medicine Keck School of Medicine University of Southern California (USC), Los Angeles, CA, United States, 3Siemens Healthcare, Los Angeles, CA, United States
Synopsis
This study evaluated CBF and BBB water exchange rate (kw) measured by diffusion prepared pseudo-continuous arterial spin labeling (DP-pCASL) in a cohort of aged African American individuals. The results showed decreasing CBF and kw with age, and higher CBF in females. Both CBF and kw were correlated with picture sequence memory test score. CBF was negatively correlated with white matter hyperintensities (WMH), free water (FW) and peak skeletonized mean diffusivity (PSMD), although age accounted for these correlations. These findings suggest the potential for CBF and kw as biomarkers of cerebral small vessel disease.
Introduction
Cerebral small vessel disease (cSVD) is the most common vascular cause of dementia, a major contributor to mixed dementia, and the cause of about one fifth of all strokes worldwide. Chronic hypoperfusion is thought to be a key mechanism of cSVD and cause of white matter hyperintensities (WMHs) on MRI (Shi et al., 2016). Recent studies suggest that dysfunction of the blood-brain barrier (BBB) contributes to the pathogenesis of cSVD, by allowing neurotoxins access to the brain and causing ionic imbalance, an inflammatory response around vessels and eventually demyelination of white matter fibers (Rosenberg et al., 2015). The goal of this study was to evaluate a noninvasive diffusion prepared pseudo-continuous arterial spin labeling (DP-pCASL) technique to concurrently measure cerebral blood flow (CBF), arterial transit time (ATT), and water exchange rate across the BBB in an aged cohort of African American individuals.Methods
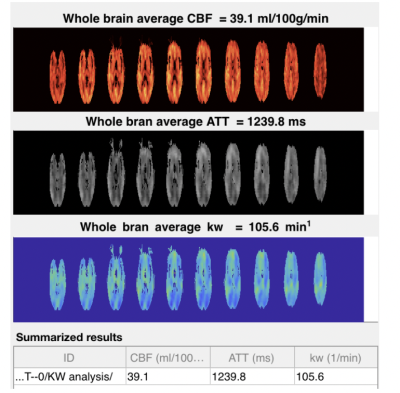
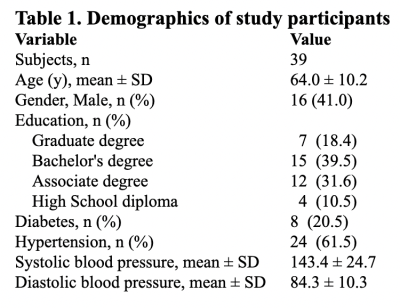
Thirty-nine African American participants with an average age of 64.0 +/- 10.2 years (16 males, 41.0%) underwent MRI on a Siemens 3T Prisma scanner. The imaging protocol included 3D T1w MPRAGE (iso-1mm resolution, ~6min); 3D T2w FLAIR (iso-1mm resolution, ~6min); 3D T2w MRI (iso-1mm resolution, ~4min); 2D diffusion tensor imaging (DTI) (iso-2mm resolution, 40 directions, b=0,1000 s/mm2, ~7min); 3D susceptibility weighted imaging (SWI) (iso-1.2mm resolution, ~5min); and DP pCASL scan with 3D GRASE readout for arterial transit time (ATT) and water exchange rate kw mapping (3.5x3.5x5mm3 resolution, PLD=900/1800ms, b=0, 50s/mm2, 10min)(Shao et al., 2019). The total scan time was ~40min. Neurocognitive assessment was performed using the NIH toolbox. DP-pCASL data were processed offline using custom Matlab toolbox to generate CBF, ATT and kw maps in each participant (Fig. 1). Public toolkits provided by the MarkVCID consortium (https://markvcid.partners.org/) were used to calculate white matter hyperintensities (WMH), mean free water (FW) and peak width of skeletonized mean diffusivity (PSMD) respectively in each participant. Linear regression models were applied to evaluate the associations of whole-brain mean CBF, ATT and kw with age, gender, cSVD biomarkers (WMH, FW, PSMD) and neurocognitive assessments using NIH toolbox, respectively.Results
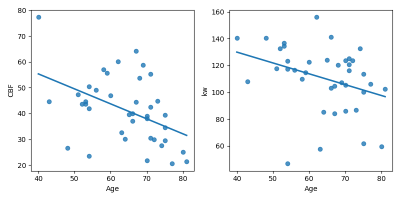
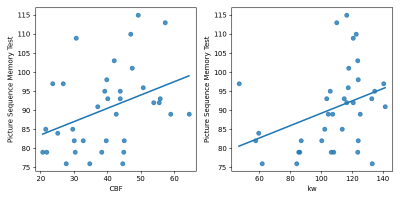
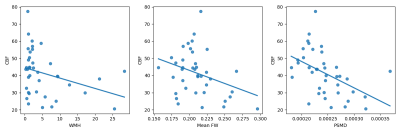
Clinical and demographic information of the cohort are summarized in Table 1. Both CBF (beta=-0.65, p=0.001) and kw (beta=-0.89, p=0.022) decrease with age (Fig. 2). ATT increased with age but the association was not significant (p=0.20). CBF was 9.4ml/100g/min higher in females than in males (p=0.013). Both CBF (beta=0.35, p=0.023) and kw (beta=0.16, p=0.034) were significantly correlated with picture sequence memory test score (Fig. 3). CBF was negatively correlated with WMH (beta=-0.6, p=0.045), mean FW (beta=-153.6, p=0.037) and PSMD (beta=-153158.9, p=0.002)(Fig. 4). However, these associations were not significant when age was included as a covariate in the regression model.Discussion
The trend of decreasing CBF and increasing ATT with age has been well recognized (Dai et al., 2017). CBF is higher in females than in males (Alisch et al., 2021), and has been shown to be associated with gross cognitive function (MoCA) and executive function in a cohort of aged Latinx subjects (Jann et al., 2021). These findings have been replicated in a cohort of aged African American individuals, who have high risks for cSVD (Castello et al., 2021). Our finding is also consistent with a recent study that reported positive associations of kw with CSF amyloid-beta42 and episodic memory score in a cohort of aged subjects with normal cognition (Gold et al., 2021). In addition, CBF was negatively correlated with existing cSVD imaging markers including WMH, FW and PSMD, although age accounted for these correlations.Conclusion
To the best of our knowledge, this is the first time that DP pCASL was applied in a cohort of aged African American individuals, who bear high risks for cSVD. Our findings suggest the potential for CBF and kw as biomarkers of cSVD, and may contribute to understanding the racial/ ethnic disparities of cSVD.Keywords
Magnetic resonance imaging, blood brain barrier, water exchange rate, arterial transit time, cerebral blood flowAcknowledgements
This study was supported by NIH grants R21EY028721 and UH3-NS100614References
Alisch, J.S.R., Khattar, N., Kim, R.W., Cortina, L.E., Rejimon, A.C., Qian, W., Ferrucci, L., Resnick, S.M., Spencer, R.G., Bouhrara, M., 2021. Sex and age-related differences in cerebral blood flow investigated using pseudo-continuous arterial spin labeling magnetic resonance imaging. Aging (Albany NY) 13, 4911-4925.
Castello, J.P., Pasi, M., Abramson, J.R., Rodriguez-Torres, A., Marini, S., Demel, S., Gilkerson, L., Kubiszewski, P., Charidimou, A., Kourkoulis, C., DiPucchio, Z., Schwab, K., Gurol, M.E., Viswanathan, A., Anderson, C.D., Langefeld, C.D., Flaherty, M.L., Towfighi, A., Greenberg, S.M., Woo, D., Rosand, J., Biffi, A., 2021. Contribution of Racial and Ethnic Differences in Cerebral Small Vessel Disease Subtype and Burden to Risk of Cerebral Hemorrhage Recurrence. Neurology 96, e2469-e2480.
Dai, W., Fong, T., Jones, R.N., Marcantonio, E., Schmitt, E., Inouye, S.K., Alsop, D.C., 2017. Effects of arterial transit delay on cerebral blood flow quantification using arterial spin labeling in an elderly cohort. J Magn Reson Imaging 45, 472-481.
Gold, B.T., Shao, X., Sudduth, T.L., Jicha, G.A., Wilcock, D.M., Seago, E.R., Wang, D.J., 2021. Water exchange rate across the blood-brain barrier is associated with CSF amyloid-beta42 and cognitive performance in healthy older adults. Alzheimer's and Dementia, (In press).
Jann, K., Shao, X., Ma, S.J., Cen, S.Y., D’Orazio, L., Barisano, G., Yan, L., Casey, M., Lamas, J., Staffaroni, A.M., Kramer, J.R., J.M., Wang, D.J., 2021. Evaluation of Cerebral Blood Flow Measured by 3D PCASL as Biomarker of Vascular Cognitive Impairment and Dementia (VCID) in a Cohort of Elderly Latinx Subjects at Risk of Small Vessel Disease. Frontier in Neurosci 15, 627627.
Rosenberg, G.A., Wallin, A., Wardlaw, J.M., Markus, H.S., Montaner, J., Wolfson, L., Iadecola, C., Zlokovic, B.V., Joutel, A., Dichgans, M., Duering, M., Schmidt, R., Korczyn, A.D., Grinberg, L.T., Chui, H.C., Hachinski, V., 2015. Consensus statement for diagnosis of subcortical small vessel disease. J Cereb Blood Flow Metab.
Shao, X., Ma, S.J., Casey, M., D'Orazio, L., Ringman, J.M., Wang, D.J.J., 2019. Mapping water exchange across the blood-brain barrier using 3D diffusion-prepared arterial spin labeled perfusion MRI. Magn Reson Med 81, 3065-3079.
Shi, Y., Thrippleton, M.J., Makin, S.D., Marshall, I., Geerlings, M.I., de Craen, A.J., van Buchem, M.A., Wardlaw, J.M., 2016. Cerebral blood flow in small vessel disease: A systematic review and meta-analysis. J Cereb Blood Flow Metab 36, 1653-1667.
Figures