4296
Diagnostic evaluation of the Kaiser scoring combined with breast vascular assessment for the characterization of breast lesions1Department of Radiology, Chengdu Women's and Children's Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, China, 2Clinical Science, Philips Healthcare, Chengdu, China
Synopsis
Kaiser scoring (KS) system for breast magnetic resonance imaging (bMRI) is a new clinical decision-making tool for the diagnosis of breast lesions. This study proposed and investigated the feasibility of Kaiser score combined with breast vascular assessment, defined as KS* , for its diagnostic performance in breast magnetic resonance imaging (bMRI). The results showed that the additional used ipsilateral breast vascularity and positive adjacent vessel sign (AVS) can accurately evaluate breast lesions, and KS* has higher diagnostic efficiency for breast lesions than conventional KS, especially for non-mass lesions.
Introduction
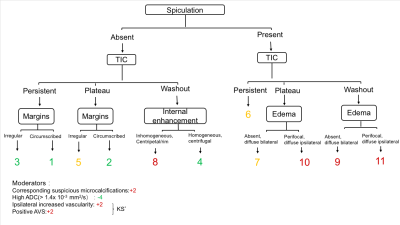
Kaiser scoring (KS) system (as shown in Figure 1) for breast magnetic resonance imaging (bMRI) is a new clinical decision-making tool for the characterization of breast lesions 1. Previous studies have demonstrated the diagnostic value and reliability of Kaiser score in the evaluation of breast lesions2-4. However, Kaiser scoring system did not include the evaluation of breast vascularity. The evaluation of blood supply of breast lesions is of great significance for the qualitative diagnosis of breast lesions. Increased ipsilateral breast vascularity and adjacent vessel sign (AVS) have been found associating with breast cancer, which indicate a poor prognosis5-7. Therefore, this study aimed to propose the using of Kaiser score combined with breast vascular assessment, defined as KS* ,and investigated its feasibility and effectiveness in the differentiation of benign and malignant breast lesions.Methods
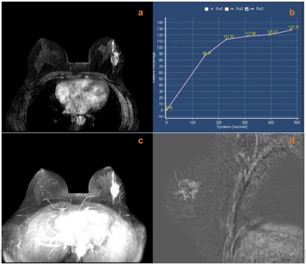
This study was approved by the institutional ethics committee. 171 patients (mean age 44.8 ± 11.4 years) with suspicious breast lesions and pathologically verified results, from May,2021 to November, 2019, were included in the retrospective study. All patients underwent breast MRI within 15 days before surgery or biopsy on a 3T MRI scanner using a dedicated 7-channel phased-array breast coil (Ingenia, Philips). The axial protocol starts with precontrast T2w-TSE, T1w-TSE, DWI, and T2w-SPAIR sequences. Axial T1-weighted dynamic sequences were measured once before and five times after contrast agent injection with a 83 sec/phase temporal resolution. Unenhanced images in the dynamic sequence were subtracted from the second series of contrast-enhanced images to generate subtracted images, and maximum intensity projections (MIPs) reconstruction was applied to the subtracted images.The Kaiser score ranges from 1 to 11(increased Kaiser score reflects increasing probabilities of malignancy, Figure 1)1. For breast vascular assessment,the vessel that has a length≥3 cm and a diameter≥2 mm was counted for the breast with lesion and its contralateral breast on MIPs images. If the number of vessels of lesion-bearing breast is higher by two or more than those in the contralateral breast, it was considered to be increased ipsilateral breast vascularity5. Adjacent vessel sign (AVS) were defined as the presence of vessels either entering the enhancing lesion or in contact with the lesion edge on subtraction images6. The diagnostic score using KS* was obtained according to the additional results of breast vascular evaluation (ipsilateral increased vascularity: +2; positive AVS, +2).The receiver operating characteristic (ROC) curve was used for comparing differences in diagnostic performance between KS* and KS, and the area under receiver operating characteristic (AUC) were calculated. The DeLong test was used for comparison of AUCs. P values < 0.05 were considered statistically significant.Results
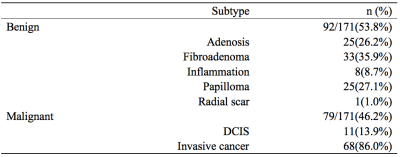
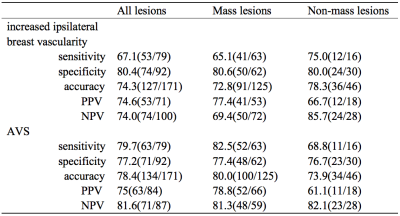
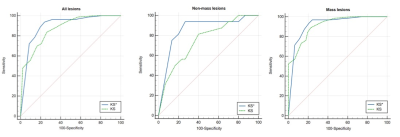
There were 92 (53.8%) benign and 79 (46.2%) malignant lesions in total. .The most common benign lesions were fibroadenoma (33,35.9%), while the most common malignant lesions were invasive cancer (68,86.0%) (Table 1). As shown in Table 2, the overall sensitivity, specificity, of ipsilateral increased vascularity associated with ipsilateral malignancy were 67.1% (53/79), 80.4% (74/92), 74.3% (127/171), respectively. The overall sensitivity, specificity, and accuracy of AVS were 79.7% (63/79), 77.2% (71/92),78.4% (134/171), respectively. The AUC analysis of KS* showed higher performance than that of KS (0.901 VS. 0.870, P=0.032)(Figure 3). The largest difference between AUC was observed when assessing non-mass subgroup (0.858 VS. 0.750, P=0.022) (Figure 2 and 3). For all lesions,KS* had a high sensitivity (92.6%) and specificity (76.1%) when a score > 7 was considered as a cut-off for malignancy.Discussion and Conclusions
This study compared the diagnostic efficacy of KS* (which was combined KS with breast vascular assessment) and KS and for breast lesions. Ipsilateral increased vascularity and AVS were significantly associated with malignancy. KS*can effectively improve the diagnostic ability of KS for breast lesions, especially for non-mass lesions.Acknowledgements
Not applicable.References
1. Dietzel M, Baltzer PAT. How to use the Kaiser score as a clinical decision rule for diagnosis in multiparametric breast MRI: a pictorial essay. Insights Imaging. 2018;9(3):325-335. doi:10.1007/s13244-018-0611-8
2. Milos RI, Pipan F, Kalovidouri A, et al. The Kaiser score reliably excludes malignancy in benign contrast-enhancing lesions classified as BI-RADS 4 on breast MRI high-risk screening exams. Eur Radiol. 2020;30(11):6052-6061. doi:10.1007/s00330-020-06945-z
3. Istomin A, Masarwah A, Vanninen R, Okuma H, Sudah M. Diagnostic performance of the Kaiser score for characterizing lesions on breast MRI with comparison to a multiparametric classification system. Eur J Radiol. 2021;138:109659. doi:10.1016/j.ejrad.2021.109659
4. Jajodia A, Sindhwani G, Pasricha S, et al. Application of the Kaiser score to increase diagnostic accuracy in equivocal lesions on diagnostic mammograms referred for MR mammography. Eur J Radiol. 2021;134:109413. doi:10.1016/j.ejrad.2020.109413
5. Sardanelli F, Iozzelli A, Fausto A, Carriero A, Kirchin MA. Gadobenate dimeglumine-enhanced MR imaging breast vascular maps: association between invasive cancer and ipsilateral increased vascularity. Radiology. 2005;235(3):791-797. doi:10.1148/radiol.2353040733
6. Han M, Kim TH, Kang DK, Kim KS, Yim H. Prognostic role of MRI enhancement features in patients with breast cancer: value of adjacent vessel sign and increased ipsilateral whole-breast vascularity. AJR Am J Roentgenol. 2012;199(4):921-928. doi:10.2214/AJR.11.7895
7. Fusco R, Sansone M, Filice S, Petrillo A. Breast contrast-enhanced MR imaging: semiautomatic detection of vascular map. Breast Cancer. 2016;23(2):266-272. doi:10.1007/s12282-014-0565-8
Figures