4295
MRI-based radiomics model for preoperative prediction of extramural venous invasion of rectal adenocarcinoma1Harbin Medical University, Harbin, China
Synopsis
Radiomics features were extracted through MRI images and different prediction models (clinical model, logistic regression [LR], random forest [RF], support vector machine [SVM], clinical-LR model, clinical-RF model, and clinical-SVM model) for extramural venous invasion (EMVI) were constructed on the basis of radiomics features and clinical factors, respectively. The optimal model, which had the best predictive efficiency, was screened out for predicting the EMVI status of rectal adenocarcinoma patients.
Introduction
Extramural venous invasion (EMVI) is defined as the appearance of tumor cells in the veins beyond the muscularis propria. EMVI status plays a vital role in the preoperative evaluation and is an independent prognostic factor of rectal cancer [1, 2]. It is relevant with local recurrence, distant metastases, and overall survival time reduction [3-5]. An accurate assessment of EMVI status is of great clinical significance for making decisions and improving the prognosis of patients.Methods
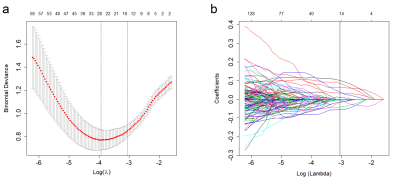
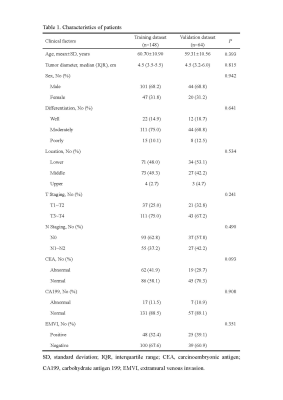
Two hundred and twelve rectal adenocarcinoma patients from September 2012 to July 2019 were included and distributed to training and validation datasets. Radiomics features were extracted from pretreatment T2-weighted images. Different prediction models (clinical model, logistic regression [LR], random forest [RF], support vector machine [SVM], clinical-LR model, clinical-RF model, and clinical-SVM model) on the basis of radiomics features and clinical factors were constructed, respectively. The area under the curve (AUC) and accuracy were used to assess the predictive efficacy of different models. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated, too.Results
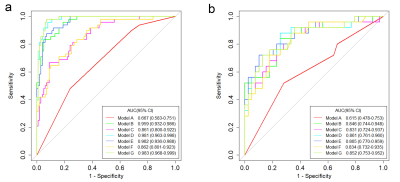
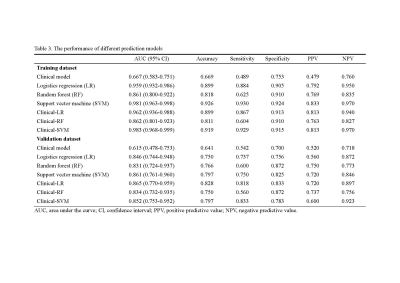
The clinical-LR model exhibited the best diagnostic efficiency with AUC of 0.962 (95% CI 0.936–0.988) and 0.865 (95% CI 0.770–0.959), accuracy of 0.899 and 0.828, sensitivity of 0.867 and 0.818, specificity of 0.913 and 0.833, PPV of 0.813 and 0.720, and NPV of 0.940 and 0.897 for the training and validation datasets, respectively.Discussion
EMVI status is an important prognostic factor of rectal adenocarcinoma. In this study, we constructed different prediction models and screened out the optimal model, which had the best performance in predicting the EMVI status. The optimal model was a multi-scale comprehensive model, and the diagnostic efficiency was good both in the training and validation datasets. As a noninvasive evaluation tool, this prediction model may provide support in clinical risk stratification.Conclusion
The radiomics-based prediction model is a valuable tool in EMVI detection and can assist decision making in clinical practice.Acknowledgements
No acknowledgement found.References
1. Ale Ali H, Kirsch R, Razaz S, Jhaveri A, Thipphavong S, Kennedy ED, et al. Extramural venous invasion in rectal cancer: overview of imaging, histopathology, and clinical implications. Abdominal radiology (New York) 2019; 44: 1-10.
2. Fournier FR, Motamedi A, Brown CJ, Phang T, Raval M, Hague CJ, et al. Oncologic outcomes associated with MRI-detected extramural venous invasion (mrEMVI) in rectal cancer: A systematic review and meta-analysis. Ann Surg 2021.
3. van den Broek JJ, van der Wolf FSW, Heijnen LA, Schreurs WH. The prognostic importance of MRI detected extramural vascular invasion (mrEMVI) in locally advanced rectal cancer. Int J Colorectal Dis 2020; 35: 1849-54.
4. Brown PJ, Hyland R, Quyn AJ, West NP, Sebag-Montefiore D, Jayne D, et al. Current concepts in imaging for local staging of advanced rectal cancer. Clin Radiol 2019; 74: 623-36.
5. Zhang XY, Wang S, Li XT, Wang YP, Shi YJ, Wang L, et al. MRI of extramural venous invasion in locally advanced rectal cancer: relationship to tumor recurrence and overall survival. Radiology 2018; 289: 677-85.
Figures