4269
Improved Differentiation of Benign and Malignant Breast Lesions with Synthetic Relaxometry and Kaiser Score1The Third Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
Early detection and accurate characterization can reduce significantly the death rates of breast cancer patients. Kaiser score (KS) demonstrates robust and wonderful performance in the assessment of breast lesions. Nevertheless, this scoring system lacks quantitative parameters, which may lead to false negatives, especially for breast cancers exhibiting atypical morphological features. In this study, the quantitative value from Synthetic MRI was added to the KS assessment to improve the differentiation of the malignant and benign breast lesions.
Introduction and purpose
Adding the quantitative synthetic relaxation times to Kaiser score (KS) may improve the diagnostic performance in the assessment of breast lesions. The aim of this study was to evaluate the differentiation performance with the combination of synthetic MRI (SyMRI) and KS for malignant and benign breast lesions.Materials and Methods
122 patients with 122 breast lesions (86 malignant and 36 benign) were included. All patients (mean age, 46.6 ± 11.6 years; age range, 18-68 years) underwent conventional MRI and SyMRI followed by DCE-MRI (SIGNA Pioneer 3T, GE Healthcare, USA). The SyMRI was acquired with TR/TE1/TE2: 7079msec/23msec/115msec, FOV: matrix: 36cm×36cm. The real and imaginary images of SyMRI were imported to SyMRI 11.0 software (Synthetic MR, Linköping, Sweden) to generate quantitative parametric maps (T1, T2, and PD maps) for further analysis. The quantitative values including T1, T2, and PD of the lesions were calculated by using the open-source software ITK-SNAP (http://www.itksnap.org/pmwiki/pmwiki.php, version 3.8). All lesions were assigned one score by using the KS system according to the study [1-3]. In this study, the lesions with high KS categories (threshold > 4) were diagnosed as malignant. If not, the lesions were diagnosed as benign [4]. All data were analyzed with the statistical software SPSS 26.0 (IBM) and MedCalc 19.8 (MedCalc Software). After the normality and homogeneity of variances were examined the quantitative SyMRI parameters (T1, T2, and PD) and KS in malignant and benign lesions were compared by using the independent sample t-test or Mann-Whitney U-test. Parameters identified to be significant after univariate analysis were conducted multivariate analysis (binomial logistic regression analysis) in further. The receiver operating characteristic (ROC) analysis was used to evaluate the diagnostic performance to differentiate malignant from benign lesions. The areas under the ROC curves (AUCs) were compared by using the Delong test. The optimal threshold, sensitivity, specificity, and accuracy were obtained at the largest Youden index. P < 0.05 was considered statistically significant.Results
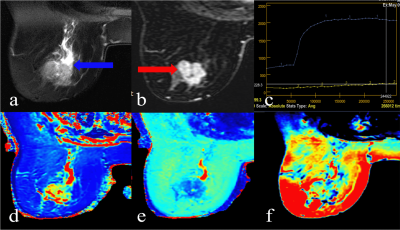
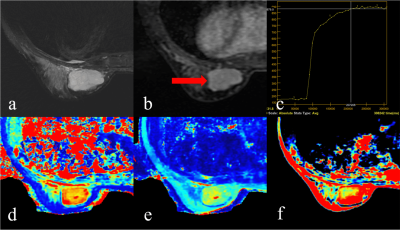
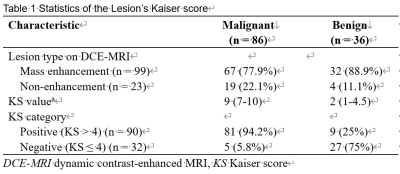
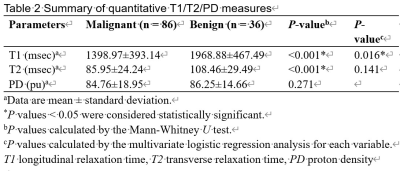
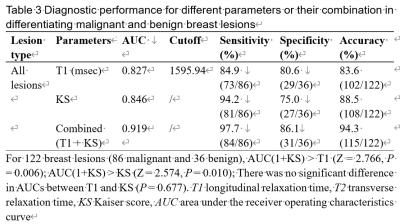
The KS of malignant lesions was significantly higher than that of benign lesions (P < 0.001). The diagnostic accuracy of the application of KS (cutoff = 4) was 88.5% (108/122) (Table 1). With Univariate analysis, significantly lower values were found in malignancy than in benign lesions for T1 (1398.97 ± 393.14 msec vs. 1968.88 ± 467.49 msec), T2 (85.95 ± 24.24 msec vs. 108.46 ± 29.49 msec), while there was no significant difference for PD. Clinical examples are provided in Figures 1-2. Multivariate analysis demonstrated that the T1 was the independent prediction factor for the risk of lesion malignant (P = 0.016) (Table 2). The ROC analysis showed the AUC of T1 (AUC = 0.827) was slightly lower than that of KS (AUC = 0.846, P = 0.677). The combination of T1 + KS demonstrated the optimal performance with AUC of 0.919, which was significantly higher than T1 (AUC = 0.827, P = 0.006) and KS (AUC = 0.846, P = 0.010). The T1 cutoff value that best distinguished malignant and benign breast lesions was 1595.94 msec. The sensitivity, specificity, and accuracy of the T1 + KS were 97.7%, 86.1%, and 94.3%, respectively (Table 3).Discussion
Kaiser score (KS) puts the independent diagnostic BI-RADS lexicon criteria into an intuitive machine-learning flowchart to grade the breast lesion in much more detail. The KS has the potential to provide higher diagnostic accuracy as well as a better inter-reader agreement in comparison with the BI-RADS lexicon [5; 6]. SyMRI with magnetic resonance imaging compilation (MAGiC) is a recently proposed multi-dynamic multi-echo (MDME) sequence, which can simultaneously generate the quantitative T1, T2, and PD maps in clinically acceptable acquisition time. The quantitative T1 and T2 are relaxation properties of tissues, which depend on the tissue components and structure, correlating with the tissue water and fat content, macromolecules concentration, and hydration state [7; 8]. With various microstructural alterations in malignant or benign lesions, the T1 and T2 values might change in a different way or degree. The mean T2 values for benign lesions (108.46 ± 29.49 msec) were found higher than those for breast cancers (85.95 ± 24.24 msec) (P < 0.001). This was in line with previous studies and the quantitative values were at the same level [9; 10]. We found that the mean T1 values of benign breast lesions (1968.88 ± 467.49 msec) were significantly higher than that of breast cancers (1398.97 ± 393.14 msec) (P < 0.001) as the same with prior reports [11; 12] while Gao et al also showed higher T1 in benign lesions but not significantly [10]. Better differentiation performance yielded in our study when combining SyMRI parameter T1 and KS than every single parameter. The AUC of the T1+KS significantly increased and the specificity also increased by 11.1% in comparison with the KS alone. What’s more, adding the T1 to the KS assessment obtained better diagnostic performance (AUC = 0.919) than the prior study with combined T1 and BI-RADS (AUC = 0.831) [13], further proving the advantage of KS in comparison with BI-RADS.Conclusion
A combination of SyMRI and KS holds the potential to improve the accuracy of diagnosis of benign and malignant lesions.Acknowledgements
The authors thank the support from the staff in the radiology department of The Third Affiliated Hospital of Zhengzhou University.References
[1] Dietzel M, Baltzer PAT. How to use the Kaiser score as a clinical decision rule for diagnosis in multiparametric breast MRI: a pictorial essay. Insights Imaging. 2018;9(3):325-335.
[2] Wengert GJ, Pipan F, Almohanna J, et al. Impact of the Kaiser score on clinical decision-making in BI-RADS 4 mammographic calcifications examined with breast MRI. Eur Radiol. 2020;30(3):1451-1459.
[3] Dietzel M, Krug B, Clauser P, et al. A Multicentric Comparison of Apparent Diffusion Coefficient Mapping and the Kaiser Score in the Assessment of Breast Lesions. Invest Radiol. 2021;56(5):274-282.
[4] Milos RI, Pipan F, Kalovidouri A, et al. The Kaiser score reliably excludes malignancy in benign contrast-enhancing lesions classified as BI-RADS 4 on breast MRI high-risk screening exams. Eur Radiol. 2020;30(11):6052-6061.
[5] Kim SJ, Morris EA, Liberman L, et al. Observer variability and applicability of BI-RADS terminology for breast MR imaging: invasive carcinomas as focal masses. AJR Am J Roentgenol. 2001;177(3):551-557.
Figures