4266
Quantitative analysis of DCE-MRI for predicting lymphovascular invasion in breast cancer1Meizhou People’s Hospital, Meizhou, China, 2Department of Radiology, Meizhou People’s Hospital, Meizhou, China, 3First Affiliated Hospital of Shantou University Medical College, Shantou, China, 4GE Healthcare, Guangzhou, China, 5Siemens Healthineers, Guangzhou, China, 6Siemens Healthineers, Shanghai, China, 7Shantou Central Hospital, Shantou, China
Synopsis
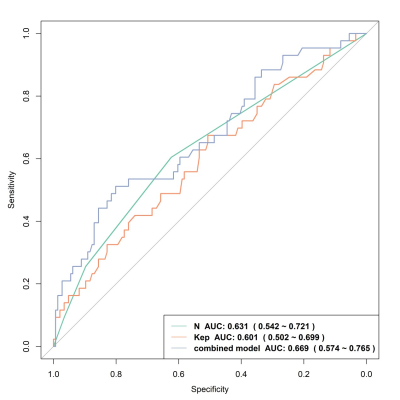
The optimal biomarkers for the diagnosis of breast lymphovascular invasion have not yet been found. DCE-MRI features can evaluate the tumor microenvironment which is related to LVI. This study explored the independent predictor of LVI, as well as developed and validated the parametric combined prediction model for the diagnosis of lymphovascular invasion in breast cancer using quantitative analysis of DCE-MRI. The prediction model based on Kep and N stage could improve the performance of LVI prediction, compared to clinicopathological or magnetic resonance parameters.
Introduction
Lymphovascular invasion (LVI) as a negative prognostic factor in invasive breast cancer (BC) can only bepostoperatively diagnosed by histopathology in clinical practice [1-2].Several studies have shown that tumor microcirculation is related to LVI, which can be non-invasive assessed using qualitative and quantitative DCE-MRI features [3-5]. Thus, the purpose of this prospective study was to determine whether quantitative parameters of DCE-MRI can preoperatively predict LVI and clinical outcome of BC patients.Methods
A total of 189 consecutive BC patients confirmed by histopathological results were enrolled in this study. All patients underwent breast MRI examinations on a 3 T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) using a 16-channel bilateral breast coil.T1-weighted volume interpolated breath-hold examination (VIBE) was first performed at two different flip angles 2° and 15° to calculate the T1-mapping images, and after the injection of gadopentetate dimeglumine (Bayer Pharma AG ), dynamic scanning with 34 consecutive phases was performed using a combination of VIBE with controlled aliasing in parallel imaging results in higher acceleration (CAIPIRINHA), view-sharing time-resolved imaging with interleaved stochastic trajectories (TWIST), and Dixon fat suppression (CAIPIRINHA-Dixon-TWIST-VIBE, CDT-VIBE) sequence. The scanning parameters of DCE-MRI included TR=6.4 ms, TE=3.34 ms, FOV=340 mm×340 mm, matrix=288×384, slice thickness=2 mm, no slice gap, flip angle 9°, temporal resolution 8.7 s, and acquisition time 305 s. Quantitative (Ktrans, Ve, Kep) and semiquantitative parameters (W-in, W-out, TTP) derived from DCE-MRI and clinicopathological features were calculated and compared between LVI-positive and LVI-negative groups. Univariate and multivariate logistic regression analysis were used to determine the prediction model for LVI. Receiver operating characteristic (ROC) curves and Kaplan-Meier curves were performed to evaluate the diagnostic efficiency of the model and the relationships with the clinical outcomes.Results
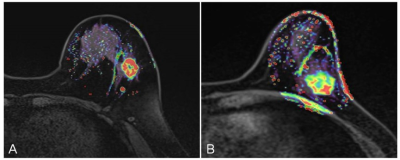
LVI-positive groups had a higher Kep value than LVI-negative groups (0.92±0.30 vs. 0.81±0.23, P=0.012), as shown in the figure 1. No significant differences were found for other parameters between patients with and without LVI (all P>0.05). N2 stage [odds ratio (OR) =3.75, P=0.018], N3 stage (OR=4.28, P=0.044) and Kep value (OR=5.52, P=0.016) were positively correlated with LVI. The combined-predicted LVI model that incorporated N stage and Kep yielded a maximum AUC of 0.669 (0.574-0.765), with a cutoff value of 0.276, accuracy of 0.735, sensitivity of 0.512, and specificity of 0.801(figure 2).Discussion & Conclusion
In the present study, we compared the clinicopathological features and parameters of DCE-MRI between LVI-positive and LVI-negative BC patients to explore the independent risk factors for LVI. Furthermore, we developed a prediction model based on these high risk factors for LVI and validated the performance of the prediction models. The combined-predicted model established by Kep and N stage could preoperatively predict LVI status, which improved the performance of LVI prediction using only clinicopathological or magnetic resonance indicators.Acknowledgements
No acknowledgement found.References
[1] Hamy AS, Lam GT, Laas E, Darrigues L, Balezeau T, Guerin J, Livartowski A, SadaccaB, Pierga JY, Vincent-Salomon A et al: Lymphovascular invasion after neoadjuvant chemotherapy is strongly associated with poor prognosis in breast carcinoma. Breast Cancer Res Treat 2018, 169(2):295-304.
[2]Invernizzi M, Corti C, Lopez G, Michelotti A, Despini L, Gambini D, Lorenzini D, Guerini-Rocco E, Maggi S, Noale M et al: Lymphovascular invasion and extranodaltumour extension are risk indicators of breast cancer related lymphoedema: an observational retrospective study with long-term follow-up. BMC cancer 2018, 18(1):935.
[3] Kim JY, Kim SH, Kim YJ, Kang BJ, An YY, Lee AW, Song BJ, Park YS, Lee HB: Enhancement parameters on dynamic contrast enhanced breast MRI: do they correlate with prognostic factors and subtypes of breast cancers? Magn Reson Imaging 2015, 33(1):72-80.
[4] Ouyang FS, Guo BL, Huang XY, Ouyang LZ, Zhou CR, Zhang R, Wu ML, Yang ZS, Wu SK, Guo TD et al: A nomogram for individual prediction of vascular invasion in primary breast cancer. Eur J Radiol 2019, 110:30-38 [5] Igarashi T, Furube H, Ashida H, Ojiri H: Breast MRI for prediction of lymphovascular invasion in breast cancer patients with clinically negative axillary lymph nodes. Eur J Radiol 2018, 107:111-118.
Figures