4265
A risk stratification scoring system for predicting axillary lymph node metastasis in breast cancer using multiparametric MRI1Meizhou People's Hospital, Meizhou, China, 2First Affiliated Hospital of Shantou University Medical College, Shantou, China, 3GE Healthcare, Guangzhou, China, 4Siemens Healthineers, Shanghai, China, 5Siemens Healthineers, Guangzhou, China, 6Shantou Central Hospital, Shantou, China
Synopsis
This study developed and validated a point-based scoring system (PSS) for stratifying the axillary lymph node (ALN) metastasis risk of breast cancer (BC) based on preoperative clinicopathological and MRI features compared with MRI-reported ALN status model and to explore its prognostic significance. The PSS in our study provides an easy tool for surgeons to assess breast cancer patients' risk for ALN metastasis prior to surgery. And the results showed that PSS had a relatively better performance than MRI-reported ALN status model (P=0.045),with a higher AUC, accuracy, and specificity, suggesting that PSS can be routinely used in axillary nodal staging.
Introduction/Purpose
The identification of axillary lymph node (ALN) metastasis is an important factor not only for prognosis but also for deciding on the treatment strategy for breast cancer[1, 2]. Many studies have attempted to use clinicopathologic or MRI features to identify the risk of ALN metastasis in breast cancer patients, but which were insufficient to change the paradigm for axillary surgical strategy [3-4].Furthermore, although prediction models using the nomogram based on a combination of clinicopathologic and MRI features performed well for identifying ALN metastasis[5], which might be time-consuming and hard to interpret. Therefore, it is necessary to develop noninvasive and more effective approaches to predict ALN metastasis to avoid unnecessary ALN dissection and SLNB, particularly among patients without any obvious evidence of ALN metastasis on clinical and imaging examinations. This study aimed to investigate the feasibility of a risk stratification scoring system developed by preoperative clinicopathological and MRI features to predict axillary lymph node metastasis in breast cancer.Method
A total of 219 BC patients were evaluated, 110 patients had non-ALN metastasis and 109 patients had ALN metastasis; 66 patients had 1 to 2 ALN metastases, and 43 patients had more than two ALN metastases. All patients were acquired by a 3 T MR system (MAGNETOM Skyra, Siemen Healthcare, Erlangen, Germany) using a 16-channel bilateral breast coil. Conventional MR examinations including a T1-weighted fast gradient echo sequence and a T2-weighted fat-suppressed turbo spin echo sequence were acquired. DWI was performed using a readout segmented echo planar imaging (RS-EPI) technique with fat suppression in the transverse plane prior to DCE-MRI. Table 1summarized the MRI protocols of the DCE-MRI and DWI. The contrast agent gadopentetate dimeglumine (Bayer Pharma AG ) at a dose of 0.2 ml/kg was given by intravenous injection at a rate of 3.0 ml/s. The clinicopathological features of the tumors were collected for analysis. The quantitative parameters of the tumors, including the volume transfer constant (Ktrans, min-1), reverse reflux rate constant (Kep,min-1) , extracellular extravascular volume fraction (Ve), rate of contrast enhancement for inflow (W-in, min-1), rate of contrast decay for outflow (W-out, min-1), time to peak enhancement after injection (TTP, min) derived from DCE-MRI, and ADC value (×10 -3 mm2/s) from DWI were calculated. A multivariate logistic regression analysis following backward stepwise selection was used to create the PSS, and the performance of which were evaluated using receiver operating characteristic curves and the Delong test.Result
Figure 1 presented one example of the measurements of MRI qualitative features from a breast cancer patient with invasive ductal carcinoma. AJCC stage, T stage, human epidermal growth factor receptor-2, estrogen receptor, maximum tumor diameter, Kep, Ve, and TTP were identified as risk factors for ALN metastasis and were assigned scores. Patients were categorized as low risk (<16.5 points), moderate risk (16.5–20.5 points), and high risk (>20.5 points). The AUCs of the PSS in the primary and validation cohorts were 0.799 and 0.713. PSS had better performance for predicting ALN metastasis than the MRI-reported ALN status model (AUC: 0.772 vs. 0.689, P= 0.045) in the total cohort (Figure 2).Conclusion
Risk stratification scoring systems have been used to guide clinical decision-making[6-7]. In this study, to develop the risk stratification scoring system, a multivariable logistic regression analysis was used to select the risk factors for ALN metastasis. We compared it to the performance of MRI-reported ALN status model in predict ALN metastasis, and explored its prognostic significance. Our results showed that PSS has good discrimination for stratifying the ALN metastasis risk of breast cancer both in the primary cohort and in the validation cohort. In terms of ALN metastasis risk, PSS had a relatively good performance compared with the MRI-reported ALN status model.Acknowledgements
No acknowledgement found.References
[1]Chang JM, Leung JWT, Moy L, Ha SM, Moon WK: Axillary Nodal Evaluation in Breast Cancer: State of the Art. Radiology 2020, 295(3):500-515.[2]Yang X, Wu L, Ye W, et al: Deep Learning Signature Based on Staging CT for Preoperative Prediction of Sentinel Lymph Node Metastasis in Breast Cancer. Acad Radiol 2020, 27(9):1226-1233.[3]Zhao M, Wu Q, Guo L, Zhou L, Fu K: Magnetic resonance imaging features for predicting axillary lymph node metastasis in patients with breast cancer. Eur J Radiol 2020, 129:109093.[4]He Z, Lan X, Tan Y, et al: Identification of Risk Factors Associated with Axillary Lymph Node Metastasis for Sentinel Lymph Node-Positive Breast Cancer Patients. J Oncol 2020, 2020:8884337.[5]Han L, Zhu Y, Liu Z, et al: Radiomic nomogram for prediction of axillary lymph node metastasis in breast cancer. Eur Radiol 2019, 29(7):3820-3829.[6]Ni-Jia-Ti MY, Ai-Hai-Ti DL, Huo-Jia AS, et al: Development of a risk-stratification scoring system for predicting lymphovascular invasion in breast cancer. BMC Cancer 2020, 20(1):94.[7]Turner BM, Gimenez-Sanders MA, Soukiazian A, et al: Risk stratification of ER-positive breast cancer patients: A multi-institutional validation and outcome study of the Rochester Modified Magee algorithm (RoMMa) and prediction of an Oncotype DX(®) recurrence score <26. Cancer Med 2019, 8(9):4176-4188.Figures
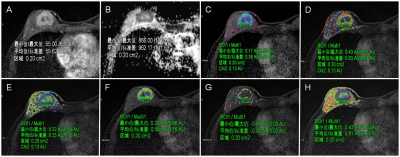
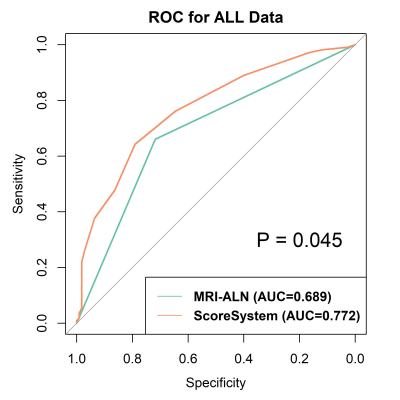
Table E1 shows the MRI acquisition parameters.
TR, repetition time; TE, echo time; TI, inversion time; FOV, field of view.