4264
stratification of axillary lymph node metastasis burden with standard breast MRI in breast cancer1Department of Radiology, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, China, 2Department of General Surgery, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, China, 3Philips Healthcare, Shanghai, China
Synopsis
Assessment of axillary lymph node metastasis burden before surgery in breast cancer patients is warranted for axillary management. This study developed a simple model based on the standard breast MRI features of breast tumor and axillary lymph node to differentiate patients with no, low or heavy axillary metastasis burden. With the help of this model, patients and clinicians would make more rational decision when to choose omitting surgery, sentinel lymph node biopsy or axillary lymph node dissection for axilla management.
Introduction
The NSABP-B32 randomized clinical trial justified the rationality of sentinel lymph node (SLN) biopsy without axillary lymph node dissection (ALND) unless any of SLNs was positive for patients with clinically negative lymph nodes1. Afterwards, the Z0011 clinical trial showed that patients with one to two positive SLNs would not obtain survival benefit from additional ALND, but may suffer from more complications, such as wound infections, axillary seromas and paresthesias2, 3, 4. Nowadays, axillary management has become more cautious in the post-Z0011 era5. Hence, accurate assessment of tumor burden in axillary lymph node (ALN) before surgery is of clinical significance to guide treatment decision making. Therefore, the aim of this study is to develop a model based on the combination of clinicopathological characteristics and MRI features of breast tumor to stratify patients by different burden of ALN metastasis in patients with breast cancer.Methods
Patients with pathological diagnosis of breast cancer from Jan. 2017 to Dec. 2019 were retrospectively reviewed. All eligible patients underwent breast surgery with SLN biopsy and/or ALND as well as breast MRI scan before surgery. Patients with zero, one to three and more than three pathologically positive lymph nodes were classified as no, low and heavy axillary metastasis burden, respectively. Preoperative factors significantly correlated with axillary burden in the univariate analysis with χ2 test were put into the ordinal logistic regression analysis to develop a predicting model. The accuracy and sensitivity of axillary burden stratification were calculated based on this model. An independent group of patients collected from Jan. 2020 to Dec. 2020 was used for validation.Results
A total of 134 female patients (median age of 60 years, range 23-77 years) were eligible for this study. Based on the number of positive ALN, 26 (19.4%), 25 (18.7%) and 83 (61.9%) patients were allocated to heavy, low and no metastasis burden, respectively. Five preoperative factors including tumor size, margin, ADC value, MRI ALN status, and time-signal intensity curve (TIC) were significantly correlated with ALN burden in the univariate analysis. A model incorporating the above five factors was developed to stratify patients with newly diagnosed breast cancer by different axillary burden, yielding the total accuracy of 73.1% (Equation 1 and 2). $$Ln[p1/(p2+p3)]=6.91+1.21X1+0.82X2+2.84X3+1.15X4+1.95X5+2.87X6$$ $$Ln[(p1+p2)/p3]=8.07+1.21X1+0.82X2+2.84X3+1.15X4+1.95X5+2.87X6$$In the equations, p1, p2 and p3 denotes the probability of no, low and heavy ALN metastasis burden respectively; X1, X2, X3, X4, X5, and X6 denotes size larger or equal than 25 mm, irregular/spiculated margin, hypointensity on ADC, MRI Suspicious ALN, plateau TIC, and washout TIC, respectively. The sensitivity to predict patients with no, low and heavy ALN burden was 96.4%, 8.0% and 61.5%, respectively. In the validation group of 57 comparable patients, this model yielded total accuracy of 82.5%, and the sensitivity to predict patients with no, low and heavy ALN burden was 94.3%, 64.3% and 62.5%, respectively.
Discussion
In order to diminish the axillary resection extent without at the expense of survival, management depending on different metastasis burden is a reasonable choice for modern therapy of breast cancer. With adequate accuracy, patients with no metastasis burden can safely avoid axillary surgery, SLNB is adequate for low burden, while direct ALND is warranted for heavy burden. When plenty of previous studies have tried to determine the ALN burden with various methods, only one published study classified patients into three groups of no, low and heavy burden based on the deep learning radiomics of conventional ultrasound and shear wave elastography6. Both this study and ours showed poor in differentiating low burden from the other two groups, indicating the limitation of MRI or ultrasound alone in predicting ALN metastasis burden. Improvement in differentiating ability is needed and may be achieved by incorporating other relevant factors, such as clinicopathological factors or combination of MRI and US results in the model, which is needed to be validated in future. Nonetheless, this model holds great promising for more appropriate choice of axilla management. Besides, small sample size of this study may limit the power of the conclusion.Conclusion
A simple model based on the standard breast MRI features including breast tumor and ALN may be helpful for the preoperative stratification of axillary metastasis burden in patients with newly diagnosed breast cancer.Acknowledgements
This study was funded by the National Natural Science Foundation of China (Grant No 81871325, 81801656).
References
1. Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11(10):927-933.
2. Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305(6):569-575.
3. Giuliano AE, Ballman KV, McCall L, et al. Effect of Axillary Dissection vs No Axillary Dissection on 10-Year Overall Survival Among Women With Invasive Breast Cancer and Sentinel Node Metastasis: The ACOSOG Z0011 (Alliance) Randomized Clinical Trial. JAMA. 2017;318(10):918-926.
4. Lucci A, McCall LM, Beitsch PD, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25(24):3657-3663.
5. Chang JM, Leung JWT, Moy L, Ha SM, Moon WK. Axillary Nodal Evaluation in Breast Cancer: State of the Art. Radiology. 2020;295(3):500-515.
6. Zheng X, Yao Z, Huang Y, et al. Deep learning radiomics can predict axillary lymph node status in early-stage breast cancer. Nat Commun. 2020;11(1):1236.Figures
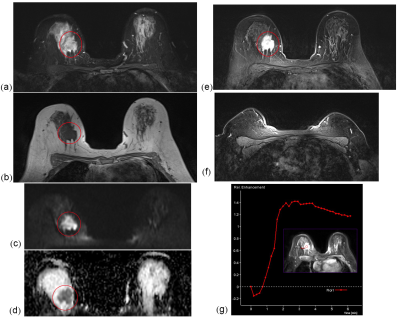
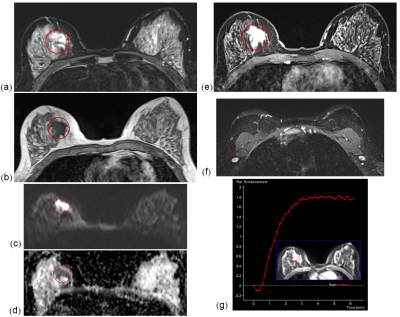
Figure 2 An example of incorrect classification of axillary burden. A unifocal lesion at the right breast of a 41-year-old female. (a)T2WI, (b)T1WI, (c)DWI, (d)ADC, (e)DCE T1WI, (g)TIC, (f)suspicious lymph node. Four positive lymph nodes were identified in postoperative specimen. The probabilities of heavy, low and no axillary burden for this patient based on the model were 36.7%, 57.3% and 6.0% respectively, and classified her as low burden, which was underestimated actually.