4256
Comparison between image quality of 3D T1 GRE sequence with and without deep learning reconstruction at gadoxetic acid-enhanced liver MRI
Jeong Hee Yoon1, Joonsung Lee2, Ersin Bayram3, and Jeong Min Lee1
1Radiology, Seoul National University Hospital, Seoul, Korea, Republic of, 2GE Healthcare, Seoul, Korea, Republic of, 3GE Healthcare, Houston, TX, United States
1Radiology, Seoul National University Hospital, Seoul, Korea, Republic of, 2GE Healthcare, Seoul, Korea, Republic of, 3GE Healthcare, Houston, TX, United States
Synopsis
Liver magnetic resonance imaging (MRI) has been widely performed for liver lesion detection and characterization. There have been attempts to improve the image quality of T1-weighted images at liver MRI. Recently, deep learning (DL)-based reconstruction gains attention as a tool for improving the image quality without substantial computational power or difficult sequence modification.
Introduction
Gadoxetic acid-enhanced liver magnetic resonance imaging (MRI) has been widely used for liver lesion detection and characterization (1). Despite the performance of gadoxetic acid-enhanced liver MRI, there is a room for image quality improvement since signal-to-noise is often compromised due to the breath-holding time. Deep-learning (DL) based reconstruction may show a way to resolve the issue at liver MRI (2). Therefore, the study purpose is to compare the image quality between conventional and deep-learning based reconstruction 3D fat-suppressed T1-weighted images at gadoxetic acid-enhanced liver MRI.Methods
In this retrospective study, consecutive patients who underwent gadoxetic acid-enhanced liver MRI a 3T scanner (SIGNATM Premier, GE Healthcare) between March 2021 and June 2021 were included. Precontrast, arterial, portal venous and hepatobiliary phases were obtained before and after standard dose of gadoxetic acid (0.025mmol/kg, Primovist, Bayer) using 3D fat-suppressed gradient echo sequence (LAVA). Arterial phase was obtained under the MR fluoroscopy guidance. Portal venous and hepatobiliary phases were obtained 65 sec and 15 min after contrast media administration, respectively. Scan parameters were as follows: TR/TE = 3.9/1.8 msec, matrix 384 x 320, slice thickness 5 mm with 2.5 mm spacing for precontrast and hepatobiliary phases. For arterial phase, TR/TE = 3.1/1.4 msec, matrix 256 x240. For portal venous phase, TR/TE 3.4/1.6, 2 mm slice thickness with 1 mm spacing, matrix 300 x 200. Field of view 380 x 380 and NEX 0.7 were applied to all sequences.DL-based Image reconstruction: The raw data of all sequences was exported, and the DL-based reconstruction was performed by offline processing. A 2D DL reconstruction algorithm (AIR Recon DL) (3), with denoising and sharpening properties, was retrained for 3D reconstruction, and was used for DL reconstruction. The network offered tunable noise reduction levels (25, 50 and 75%; higher levels indicated higher levels of denoising) and a factor of 75% was chosen for this study.
Image analysis: Two board-certified radiologists evaluated the image quality of precontrast, arterial, portal venous and hepatobiliary phases in consensus. Image noise, motion artifact, ringing artifact and overall image quality were assessed on a five-point scale in which higher score indicates better image quality and less artifacts. In addition, hepatic artery, portal vein and hepatic vein conspicuity was assessed on arterial, portal and hepatobiliary phases. Lastly, liver margin was assessed on portal venous and hepatobiliary phases.
Results
Thirty patients were included (male = 18, mean age 69 ± 11 years). Regarding the overall image quality, DL-based reconstruction images showed significantly better image quality in precontrast (3.1 ± 0.5 vs. 4.3 ± 0.9), arterial (2.7 ± 0.6 vs. 3.9 ± 1.1), portal (3.6 ± 0.5 vs, 4.3 ± 0.8), hepatobiliary (3.2 ± 0.6 vs. 4.1 ± 1.0) phases (P < 0.001 for all). Image noise was significantly lower in DL-based reconstruction images on precontrast (2.9 ± 0.5 vs. 4.8± 0.4), arterial (2.7 ± 0.6 vs. 3.9 ± 1.1), portal venous (2.9 ± 0.4 vs. 4.7 ± 0.5) and hepatobiliary (3.7 ± 0.6 vs. 4.8 ± 0.4) phases (P < 0.001 for all) (Fig 1). Ringing artifact was also decreased in all phases (P < 0.001) except arterial phase (4.1 ± 0.8 vs. 4.2 ± 0.5, P = 0.35) (Fig 2). Sharper liver margin was observed on DL-reconstructed portal venous (3.8 ± 0.4 vs. 4.5 ± 0.7) and hepatobiliary (3.7 ± 0.5 vs. 4.5 ± 0.7) phases (P < 0.001 for all). Motion artifact was slightly improved on precontrast (4.0 ± 0.7 vs. 4.6 ± 0.7, P = 0.003), arterial (3.2 ± 1 vs. 4.0 ± 1.1, P = 0.005) whereas no difference of motion artifact was observed on portal venous (4.1 ± 0.7 vs. 4.4 ± 0.4, P = 0.1), hepatobiliary (4.1 ± 0.8 vs. 4.5 ± 0.7, P = 0.06) phases. Hepatic artery conspicuity (3.4 ± 1.1 vs. 4.1 ± 1.1, P = 0.16), portal vein conspicuity (4.0 ± 0.4 vs. 4.8 ± 0.4, P < 0.001) and hepatic vein conspicuity (3.5 ± 0.8 vs. 4.1 ± 1.0, P = 0.015) were also significantly higher on DL-based reconstructed images.Conclusion
DL-based reconstruction provided better image quality compared with conventional fat-suppressed T1 GRE sequences by lowering image noise and artifacts.Acknowledgements
No acknowledgement found.References
1. Lee YJ, Lee JM, Lee JS, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology 2015;275(1):97-109. doi: 10.1148/radiol.14140690 2. Tajima T, Akai H, Sugawara H, et al. Breath-hold 3D magnetic resonance cholangiopancreatography at 1.5 T using a deep learning-based noise-reduction approach: Comparison with the conventional respiratory-triggered technique. Eur J Radiol 2021;144:109994. doi: 10.1016/j.ejrad.2021.109994 3. Lebel RM. Performance characterization of a novel deep learning-based MR image reconstruction pipeline; arXiv preprint arXiv:200806559. 2020Figures
Figure
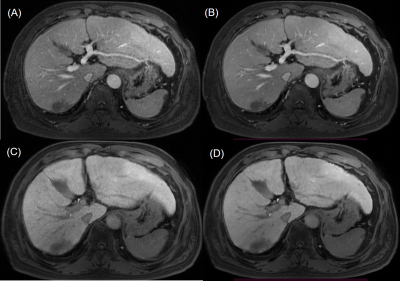
1. A 59-year-old male with chronic hepatitis. Compared with conventional portal
venous phase (A) and hepatobiliary phase (C), deep learning (DL)-based
reconstructed portal venous (B) and hepatobiliary phases (D) showed less noise,
sharper liver margin and better portal and hepatic vein conspicuity.
Figure
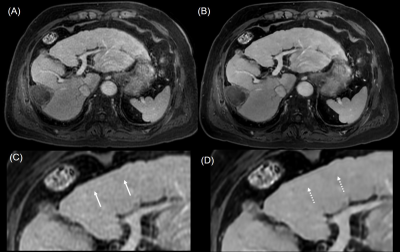
2. A 79-year-old man with chronic hepatitis. Compared with conventional portal
venous phase (A), DL-based reconstructed portal venous phase images (B) showed
less image noise and slightly sharper liver margin and better portal vein
conspicuity. In addition, ringing artifact on portal venous phase (C, arrows)
also decreased on DL-based reconstructed images (D, dotted arrows).
DOI: https://doi.org/10.58530/2022/4256