4240
The Value of Clinical application of T2WI with CSAI - a deep learning constrained Compressed SENSE reconstruction on prostate cancer1Radiology department, First Hospital of JiLin University, ChangChun, China, 2Philips Healthcare, BeiJing, China
Synopsis
Image quality of T2WI suffers from long scanning time. Compressed SENSE (C-SENSE) allow for Shorter scanning time and Ensuring good image quality,Image quality can be further optimized with CSAI . A total of 20 patients with prostate cancer (PC) underwent MRI including T2WI with SENSE-2(S2)and SENSE-4 (S4)、CS4 and CSAI4. SNR was significantly higher in CSAI4 than CS4 and S4. In comparison CNR between of S4、CS4 and CSAI4 of clinically insignificant PC, only CSAI4 had significant difference. CSAI4 improves the image quality and may contribute to increased diagnostic performance of tumor and clinicians’ confidence in the detection and diagnosis of prostate cancer.
Introduction
T2WI imaging is key components of prostate multiparametric MRI (mpMRI) in patients with prostate cancer (PCa) that contributes to tumor detection, Currently, T2WI is routinely performed using the Turbo Spin Echo imaging (TSE) technique. High image resolution is a prerequisite for clear visualization of prostate cancer, however, it prolongs scan time. Compressed-SENSE (CS) reduces acquisition time by using the sparsity of MR images to randomly undersample the k-space1-3. More recently, integrating artificial intelligence (AI) into CS reconstruction has attracted much attention. Compressed SENSE-AI, based on Adaptive-CS-Net, clearly reduces noise artifacts and significantly improves the accuracy4-5,allow for a reduction of the noise and scanning time on the premise of ensuring image quality. Therefore, T2WI with CSAI may improve SNR and has potential for clinical application for tumor detection using in PC. Thus, the aim of this study is to evaluate the image quality of CSAI and compared with conventional SENSE and CS technique.Materials and Methods
total of 20 patients with ultrasonography guided prostate-targeted biopsy (UGB) with or without prostatectomy proven PCa (mean age, 71years; range, 40-89 years),including 2 tumors with Gleason Score(GS) 3+3, 6 tumors with GS 3+4, 7 tumors with GS 4+3, 1 tumor with GS 4+4 and 4 tumors with GS 4+5. Axial T2WI images were acquired by CS and CSAI with acceleration factors (AF) of 4 (CS4, CSAI4) and by conventional SENSE with AF of 4 and 2(S2 and S4, S2 as a reference scan) on a 3-T system with a 32-channel phased-array coil (Ingenia Elition 3.0T; Philips Healthcare, Best, The Netherlands) before prostate biopsy.The imaging parameters described in as follows:TR=4000ms,TE=110ms, FOV: 200mm*200mm*39mm, VOXEL:0.75mm*0.75mm*2mm, MATRIX: 268*257*18slices, default: 0.2mmm, NSA:1, Slicethickness: 2mm;total acquisition time=2min30s(S2) or 1min4s(S4) or 1min12s(CS4 and CSAI4).The signal intensity(SI) and standard deviations(SD) values were measured respectively in normal peripheral zone(PZ)、lesion and internal obturator muscle area. Then, the signal-to-noise ratio (SNR) of the normal peripheral zone and lesion area was calculated with the following formula 1: $$SNR_{tissure1}=\frac{SI_{ROI1}}{SD_{ROI1}} [1]$$The contrast-to-noise ratio (CNR) between lesion and muscle was evaluated with the formula 2: $$CNR_{tissure1-tissrue2}=\frac{|SI_{ROI1}-SI_{ROI2}|}{\sqrt{SD_{ROI1}^{2}+SD_{ROI2}^{2}}} [2]$$SNR, and CNR were compared between T2WI S2 、T2WI S4、T2WI CS4 and T2WI CSAI4,one-way repeated-measures analysis of variance (ANOVA) and post hoc Tukey test were used for statistical analysis by Graphpad 9.0. Values of P < 0.05 were considered statistically significant.Results
The overall image results of the T2WI scans using CSAI were considered sufficient for routine clinical practice, and CSAI clearly reduced the noise which exists in the background of the SENSE and CS images as exampled in Fig.1All of the SNR and CNR values of S4 sequence were significant lower than reference S2 sequence(all P<0.0001). No difference was found for the SNR of normal peripheral zone, the SNR of lesion and the CNR between lesion and normal PZ in comparison to the standard S2, CS4 and CSAI4 (p>0.05). However , the CNR between lesion and muscle of CSAI4 were significantly higher than S2 and CS4(4.96 ± 1.84 vs. 4.51 ± 1.76, P < 0.05 and 4.96 ± 1.84 vs. 4.58 ± 1.59, P <0.001). ( in Figure 2).Discussion
In the comparison of image quality using CNR and SNR, CSAI4 was higher in CS. These results suggest that CSAI has image quality that can be applied clinically, which is expected to improve detection ability of small PCa. These results are expected the usefulness of CSAI derived from CS for not only PC detection but also shorten scanning time which could enhance clinicians’ confidence in the detection and diagnosis of prostate cancer. The present results may need further validation in prospective studies with a larger number of patients and different acceleration factors.Conclusion
The present findings suggest that compared with CSAI4 and S2、S4、CS4, CSAI4 improves CNR and may contribute to increased diagnostic performance of tumor in PC. CSAI4 is more conducive to enhancing the contrast between background and lesions, and is conducive to the detection of lesions.Acknowledgements
no acknowledgement found.References
1. Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2. 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76(3):340-351.
2. Epstein JI, Egevad L, Amin MB, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: De nition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol 2016;40(2):244-252.
3. Langer DL, et al. Prostate cancer detection with multi-parametric MRI: logistic regression analysis of quantitative T2, diffusion-weighted imaging, and dynamic contrast-enhanced MRI. Magn Reson Imaging. 2009 Aug;30(2):327-34.
4. Knoll F, et al. Advancing machine learning for MR image reconstruction with an open competition: Overview of the 2019 fastMRI challenge. Magn Reson Med. 2020;(January):mrm.28338.
5. Pezzotti N, et al. Adaptive-CS-Net: FastMRI with Adaptive Intelligence. arxiv. 2019;(NeurIPS).12. Yoneyama, et al. Noise Reduction in Prostate Single- Shot DW-EPI utilizing Compressed SENSE Framework. Proc Intl Soc Mag Reson Med. 2019;27:1634
Figures
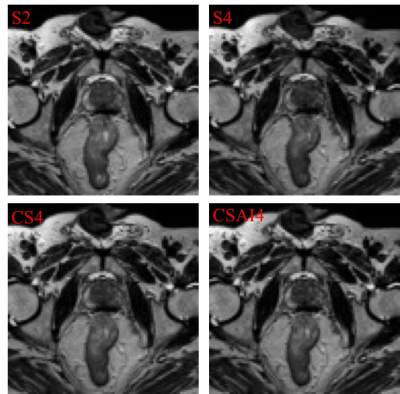
S2, S4, CS4 and CSAI4 images are respectively. It can be seen that there is a bar artifact in the upper left of prostate in the S4 image, while CS4 and CSAI4 artifacts are not shown. The contrast between CSAI4 prostate lesions and normal tissues is enhanced, and the contrast noise ratio is increased.
