4238
A comparative study of non-PTX‑zoom‑DWI with conventional DWI in bladder cancer lesion display and muscular invasion diagnosis1China-Japan Union Hospital of Jilin University, Changchun, China, 2Radiology, China-Japan Union Hospital of Jilin University, Changchun, China, 3MR Scientific Marketing, Siemens Healthineers, Beijing, China, 4Jilin Metering Center, State Grid Corporation of China, Changchun, China, 5College of Mathematics of Jilin University, Changchun, China, 6MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
The value of non-parallel-transmission zoom-diffusion weighted imaging (non-PTX zoom-DWI) compared with conventional DWI in the diagnosis of bladder cancer muscular invasion is investigated. Results show that non-PTX zoom-DWI improves sensitivity, specificity, positive predictive value, negative predictive value, and accuracy. Additionally, it has good diagnostic consistency across different readers, and shows better display of bladder than conventional DWI sequence. Non-PTX zoom-DWI may be superior to conventional DWI in predicting the muscular invasion in bladder cancer.
Introduction
Determining the depth of muscle invasion in bladder cancer is of great importance to treatment options and prognosis. Morphological MRI and diffusion-weighted imaging (DWI) has shown promising results for determining the depth of invasion.[1] However, conventional bladder DWI (con-DWI) is susceptible to artifacts due to the influence of intestinal gas and bladder urine. The purpose of this study was to compare non‑parallel‑transmission‑zoom‑DWI (non-PTX zoom-DWI) with con-DWI in bladder cancer lesion display and to investigate the value of non-PTX zoom-DWI in the diagnosis of muscular invasion in bladder cancer lesions.Methods
A total of 34 patients (29 males and 5 females; mean age, 64.6±10.6 years; 54 lesions) with bladder cancer confirmed by pathology were enrolled in this study. All the subjects underwent MRI scanning including 3D SPACE T2WI, conventional-DWI, and a prototypical non-PTX zoom-DWI on a 3T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). Conventional-DWI sequence parameters were: TR/TE=5400/70ms, FOV=240x183.4mm2, TA=4min05s. Non-PTX zoom-DWI sequence parameters were: TR/TE=4600/86ms, FOV=158x88.5mm2, TA=3min15s, Common sequence parameters were: slice thickness 3.5 mm, slice gap 0 mm, matrix size 100x100, b= 50,1000s/mm2. Two radiologists with 3 and 6 years of experience independently evaluated the T stage (AJCC) of bladder cancer, the degree of muscular layer tumor invasion, muscular layer invasion diagnostic confidence, and the overall quality of conventional DWI and non-PTX zoom-DWI images. To evaluate the presence of artifacts (in-folding, ghosting, susceptibility, blurring, etc.), the artifacts of both DWI sequences were rated visually on a five-point scale: 1, pronounced artifact, edge blur; 2, pronounced artifact, local blur; 3, moderate artifact, slightly fuzzy; 4, mild artifact, no blur; and 5, excellent image quality. After 2 weeks, the same image quality analysis was repeated by the two readers in a different order. Muscle-invasiveness diagnostic confidence was scored with 1-4 points (no, low, possible, certain). Statistical analyses were performed using SPSS (IBM, Armonk, NY, USA) for con-DWI and non-PTX zoom-DWI to evaluate the sensitivity, specificity, positive predictive value, negative predictive value, accuracy, and Youden index of bladder cancer invasion. Chi-square test was used to test for differences between the two examination methods, and the consistency test of tumor t stage and diagnosis of invasion muscle layer was used for the subjective score. Wilcoxon test was used to evaluate the subjective score. Bilateral p < 0.05 were considered significant.Results
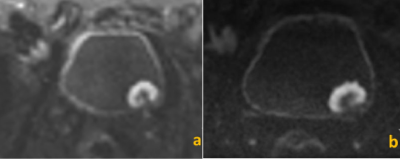
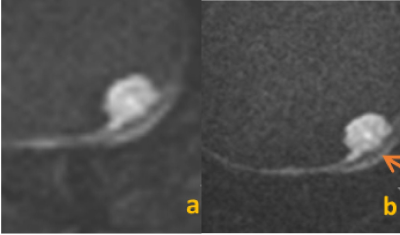
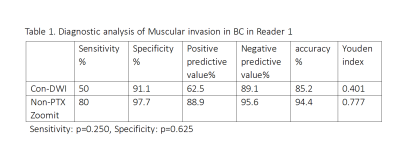
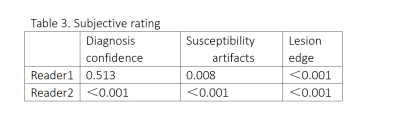
In 54 bladder cancer lesions, 10 lesions were muscular invasion, and 44 lesions were non-invasive muscular layer. Example qualitative DWI results for each technique are shown in tumors of two patients (Figures 1 and 2). Quantitatively, Reader1 (senior radiologist, Table 1) showed improved diagnostic ability with non-PTX zoom-DWI in muscle invasion of bladder cancer than with con-DWI, yet there was no statistically significant difference in sensitivity and specificity between the two methods (sensitivity, p=0.250, specificity, p= 0.625). Reader2 (junior radiologist, Table 2) had higher specificity, negative predictive value, and accuracy in DWI combined with non-PTX zoom-DWI muscle layer infiltration than con-DWI, but there was no statistically significant difference in sensitivity and specificity between the two methods (sensitivity, p=0.500, specificity, p=0.250). In terms of diagnosis of T stage, there was no difference between the two radiologists in con-DWI and non-PTX zoom-DWI, with moderate consistency (p =0.097 vs 0.264 kappa=0.534 vs 0.440), and no difference in diagnosis of bladder cancer muscle invasion. Table 3 displays the subjective rating results. Reader2 diagnosed non-PTX zoom-DWI with more confidence in muscle invasion than con-DWI (p<0.001). Con-DWI and non-PTX zoom-DWI images have significant differences in subjective score of lesion edge sharpness (reader1 p<0.001 vs reader2 p<0.001), and subjective score of susceptibility artifacts severity (Reader1 p= 0.008 vs Reader2 p<0.001).Discussion
This study investigated the advantage of non-PTX zoom-DWI in displaying bladder cancer lesions, which may improve diagnostic confidence compared with conventional-DWI. Diagnostic indexes of non-PTX zoom-DWI were higher. Although there was no statistical significance, there were only a small number of included patients with tumors above T2 stage. In clinical practice, variable techniques including T2WI and DWI images have been applied for local staging. T2WI images have high diagnostic value for luminal growth and flattening lesions but are likely to be misdiagnosed as muscular infiltration when there is intramural thickening; DWI has high differential significance [3]. Furthermore, the morphology of the reactive tumor in DWI may be a diagnostic imaging of muscular invasion [4]. Future work will increase the number of patients and analyze the diagnostic efficacy of different stages.Conclusion
Non-PTX zoom-DWI reduces susceptibility artifacts and shows better visualization of lesion edges in bladder cancer than conventional-DWI. Non-PTX zoom-DWI has potential value in the diagnosis of muscle invasion in bladder cancer.Acknowledgements
No acknowledgement found.References
[1]. Wang HJ, Pui MH, Guan J, et al. Comparison of Early Submucosal Enhancement and Tumor Stalk in Staging Bladder Urothelial Carcinoma. Am. J. Roentgenol. (2016) Aug 1-7.
[2]. Lei Hui,Liming Wei,et al.(2021)Better lesion conspicuity translates into improved prostate cancer detection:comparison of non-[arallel-transmission-zoomed-DWI with conventional-DWI,Abdominal Radiology.
[3]. Denis Séguier, Philippe Puech, Ronald Kool, Léa Dernis, Héléna Gabert, Wassim Kassouf, Arnauld Villers and Gautier Marcq.Multiparametric magnetic resonance imaging for bladder cancer: a comprehensive systematic review of the Vesical Imaging Reporting and Data System (VI-RADS) performance and potential clinical Applications,Therapeutic Advances in Urology2021; 13: 1–17.
[4]. Abdul Razik, Chandan J. Das, Sanjay Sharma, Amlesh Seth, Deep N. Srivastava, Sandeep Mathur,Rakesh Kumar, Arun K. Gup.Diagnostic performance of diffusion-weighted MR imaging at 3.0 T in predicting muscle invasion in urinary bladder cancer: utility of evaluating the morphology of the reactive tumor stalk,Abdom Radiol (2018)
Figures