4236
Reduced field-of-view diffusion-weighted MRI improving diagnostic value in cervical cancer
Huihui Wang1 and Jianxing Qiu1
1Peking University First Hospital, Beijing, China
1Peking University First Hospital, Beijing, China
Synopsis
This study was aimed to investigate the image quality and signal intensity (SI) of reduced field-of-view (r-FOV) DWI in patients with cervical cancer in comparison with full FOV (f-FOV) DWI. The subjective image quality, quantitative tumor conspicuity and quantitative normal tissue contrast were better for the r-FOV DWI images than for f-FOV DWI. The tumour diameters measured from the r-FOV DWI images experienced less bias than those from the f-FOV DWI. Those suggest that r-FOV DWI improving diagnostic value in cervical cancer than f-FOV DWI.
Purpose
Magnetic resonance imaging (MRI) plays an important role in the evaluation of tumor size and local infiltration of cervical cancers. Diffusion-weighted imaging (DWI) with reduced field-of-view (FOV) has been shown to provide high spatial resolution with reduced distorsion in the spinal cord, breast, pancreas, and prostate gland. This study was aimed to evaluate the image quality and and compare the signal intensity (SI) of reduced field-of-view (r-FOV) DWI (b=1000 s/mm2) in patients with cervical cancer in comparison with full FOV (f-FOV) DWI (b=1000 s/mm2).Method
This study was approved by the institutional review board. Twenty-eight patients diagnosed with cervical cancer and thirty patients diagnosed without cervical cancer by pathology were prospectively included. Female pelvic magnetic resonance imaging was performed using a 3T magnetic resonance scanner. All pelvic MRI sequences included f-FOV DWI (b=1000 s/mm2) and r-FOV DWI (b=1000 s/mm2) before therapy. Two radiologists independently rated image quality for r-FOV DWI and f-FOV DWI regarding anatomic detail, lesion conspicuity (only for patients with cervical cancer), presence of artifacts, and overall image quality using the following 5-point scale. The scores were compared using Wilcoxon signed-rank test. Interobserver agreement was evaluated by weighted κappa statistics. The agreement was interpreted as follows: poor (κ < 0.20); fair (κ = 0.21-0.40); moderate (κ = 0.41-0.60); good (κ =0.61-0.80); and very good (κ = 0.81-1.00). For patients with cervical cancer, the SI of the tumour tissue and normal cervical sroma were measured at two DWI sequences. If normal cervical tissue was destroyed by tumor, then SI of normal uterus corpus tissue was measured. For patients without cervical cancer, the SI of the cervical endometrium and cervical stroma was measured at the two DWI sequences. CNRcervical cancerwas defined as (SItumor – SIstoma) / (SItumor + SIstroma) and CNRnormal tissuewas defined as (SIendometrium– SIstroma) / (SIendometrium+ SIstroma). To measure the SI, regions of interest (ROIs) were independently drawn to encompass the tumour lesions with hyperintense signal on the images by each reader. The ROIs were copied for two DWI sequences. The T2WI was referenced to ensure that the identical tumour areas and normal cervical tissue areas were measured in two DWI sequences. Additionally, the SI contrast ratios were calculated and compared using the Mann-Whitney U test, the ADC values of tumours and the maximum tumour diameters were measured from two DWI sequences and compared with those from the T2WI, which was the reference standard. The distribution and concordance of the maximum lesion diameters were shown in a Bland-Altman plot.Result
Results: The anatomic detail, lesion conspicuity, presence of artifacts, and overall image quality quality scores were higher for the r-FOV DWI than for f-FOV DWI (P=0.001~0.031, Table 1). The interobserver agreement was fair to excellent for anatomic detail, lesion conspicuity, presence of artifact, and overall image quality (κ = 0.478 – 0.931 at r-FOV DWI and κ = 0.457 – 0.916 at f-FOV DWI images, Table 2). The CNR cervical cancerwere higher for the r-FOV DWI than for the f-FOV DWI sequences (0.50 ±0.14 vs 0.42 ±0.15, P = 0.024). The CNRnormal tissuewere also higher for the r-FOV DWI than for the f-FOV DWI (0.39 ±0.1 vs 0.33±0.08, P = 0.004, Figure 1 and 2). There was no significant difference in mean tumor ADC value between the two DWI sequences (826.1 ± 78.4 mm2/s at r-FOV DWI vs 849.5 ± 106.3 mm2/sat f-FOV DWI, P = 0.085). The tumour diameters measured from the r-FOV DWI experienced less bias than those from the f-FOV DWI.The mean maximum diameter of the 28 lesions measured from the r-FOV DWI and f-FOV DWI were 32.6 ± 10.0 mm and 33.8 ± 10.2 mm.Figure 3 shows the Bland–Altman plots of the distribution and concordance of the maximum diameters of the lesions obtained on DWI and T2WI.The r-FOV DWI and T2WI had a mean difference of -0.6 ± 1.5 mm, with 95% limits of agreement ranging from -3.6 to 2.4 mm. Separately, the f-FOV DWI and T2WI had a mean difference of -0.3 ± 1.2 mm, with 95% limits of agreement ranging from -2.7 to 2.2 mm.Discussion and Conclusion
r-FOV DWI are technically feasible to acquire and show better image quality in terms of anatomic detail and lesion conspicuity with fewer artifacts than f-FOV DWI of the female pelvis. This could help radiologists to better assess cervical cancer in detail.Acknowledgements
Reduced FOV DWI may enhance diagnostic performance for evaluation of cervical cancer.References
1. Park JJ, Kim CK, Park SY, et al. Parametrial invasion in cervical cancer: fused T2-weighted imaging and high-b-value diffusion-weighted imaging with backgroundbody signal suppression at 3 T. Radiology 2015, 274: 734-741. 2. He M, Xu J, Sun Z, et al. Prospective Comparison of Reduced Field-of-View (rFOV) and Full FOV (fFOV) Diffusion-Weighted Imaging (DWI) in the Assessment of Insulinoma: Image Quality and Lesion Detection. Acad Radiol. 2020,27(11):1572-1579.3. Fournier LS, Bats AS, Durdux C. Diffusion MRI: Technical principles and application to uterine cervical cancer. Cancer Radiother. 2020,24(5):368-373.4. Exner M, Kühn A, Stumpp P, et al. Value of diffusionweighted MRI in diagnosis of uterine cervical cancer: a prospective study evaluating the benefits of DWI compared to conventional MR sequences in a 3T environment. Acta Radiol 2016,57: 869–877.5. Hwang J, Hong SS, Kim HJ, et al. Reduced field-of-view diffusion-weighted MRI in patients with cervical cancer. Br J Radiol. 2018,91(1087):20170864.6. Qi YF, He YL, Lin CY, et al. Diffusion-weighted imaging of cervical cancer: Feasibility of ultra-high b-value at 3T. Eur J Radiol. 2020,124:108779.7. Balcacer P, Shergill A, Litkouhi B. MRI of cervical cancer with a surgical perspective: staging, prognostic implications and pitfalls. Abdom Radiol (NY). 2019,44(7):2557-2571.Figures
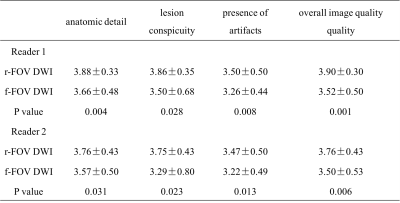
Table 1. Comparison of qualitative analysis scores between r-FOV DWI and f-FOV DWI
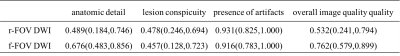
Table 2. Interobserver agreement for qualitative analysis scores
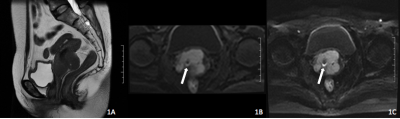
Figure 1. A 54-year-old female with squamous cell carcinoma of the cervix. (A) Sagittal T2WI. (B) Axial r-FOV DWI. (C) Axial f-FOV DWI. The suppression effect of the half-moon-shaped high-signal artifact is better at r-FOV DWI than f-FOV DWI (white arrow).
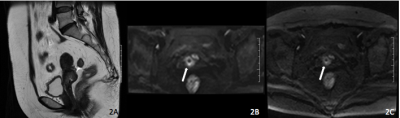
Figure 2. A 52-year-old female with squamous cell carcinoma of the cervix. (A) Sagittal T2WI. (B) Axial r-FOV DWI. (C) Axial f-FOV DWI. r-FOV DWI shows better image quality in terms of lesion conspicuity than f-FOV DWI (white arrow).
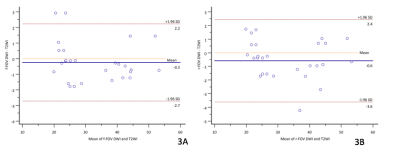
Figure 3. Bland–Altman plots of the distribution and concordance of the maximum diameters of the lesions obtained on DWI and T2WI. (A) Difference vs. average of maximum diameters: r-FOV DWI and T2W image/mm. (B) Difference vs. average of maximum diameters: f-FOV DWI and T2W image/mm
DOI: https://doi.org/10.58530/2022/4236