4230
Vascular Involvement and Resectability of Pancreatic Ductal Adenocarcinoma on Contrast-Enhanced MRI: Comparison with Pancreatic Protocol CT
Yoshifumi Noda1, Nobuyuki Kawai1, Avinash R. Kambadakone2, Tetsuro Kaga1, Takuma Ishihara3, Fuminori Hyodo4, Hiroki Kato1, and Masayuki Matsuo1
1Department of Radiology, Gifu University, Gifu, Japan, 2Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 3Innovative and Clinical Research Promotion Center, Gifu University Hospital, Gifu, Japan, 4Department of Radiology, Frontier Science for Imaging, Gifu University, Gifu, Japan
1Department of Radiology, Gifu University, Gifu, Japan, 2Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 3Innovative and Clinical Research Promotion Center, Gifu University Hospital, Gifu, Japan, 4Department of Radiology, Frontier Science for Imaging, Gifu University, Gifu, Japan
Synopsis
MRI is used as a problem-solving tool when contrast-enhanced CT is not available for assessing pancreatic ductal adenocarcinoma. In this study, we evaluated the diagnostic performance of vascular involvement and resectability on MRI and compared them with pancreatic protocol CT. Our results showed that no statistical difference in terms of the detection of vascular involvement and the resectability classification based on the NCCN guideline between CT and MRI.
Introduction
MRI is not a main imaging modality for the assessment of pancreatic ductal adenocarcinoma (PDAC); however, it is used as a problem-solving tool when contrast-enhanced CT is not available. The purpose of this study was to compare the diagnostic performance for the detection of vascular involvement and the determination of resectability differences regarding PDAC between contrast-enhanced CT and MRI.Materials and Methods
This retrospective study was approved by our Institutional Review Board, and written informed consent was waived. Between January 2008 and March 2021, 83 consecutive patients with pathologically proven PDAC who underwent both pancreatic protocol dynamic contrast-enhanced CT and MRI before surgery were included. All images analyzed in this study were obtained before surgery even in patients who had received neoadjuvant therapy. Two radiologists independently categorized the vascular involvements for the celiac, superior mesenteric, splenic, and common hepatic arteries, and for the portal, superior mesenteric, and splenic veins in the following categories: no tumor contact, solid soft-tissue contact ≤180°, or solid soft-tissue contact >180°. Vascular involvement was defined as positive when imaging findings, included solid soft-tissue contact >180°, narrowing, or occlusion. Furthermore, the radiologists also independently classified the resectability of PDAC as resectable, borderline resectable, or locally advanced based on the NCCN guidelines [1]. The reference standard for confirmation of arterial invasion was based on histopathological findings (n = 71) or surgical records (n = 11). To evaluate the diagnostic performance for the detection of vascular invasion both on CT and MRI, receiver operating characteristic (ROC) curves and areas under the ROC curves (AUCs) were calculated. The frequencies of evaluated vascular involvements and resectability were compared between CT and MRI based on the Fisher’s exact test. A P value <.05 was considered statistically significant.Results
Vascular involvements were pathologically revealed in two celiac arteries, two superior mesenteric arteries, seven splenic arteries, four common hepatic arteries, 11 portal veins, five superior mesenteric veins, and 12 splenic vein cases. We found no differences in the frequency of vascular involvement between patients treated with and without neoadjuvant therapy (P = .10–>.99). The AUCs for diagnosing vascular involvement on CT and MRI are shown in Table 1. The AUCs for diagnosing involvement of all vasculatures were not statistically different (P = .06–>.99) (Figure 1). The evaluated resectability and R0 resection rate on CT and MRI are summarized in Table 2. We found no difference in the frequency of resectability between CT and MRI (P = .15–>.99).Discussion
The preferred imaging modality for the assessment of PDAC is the pancreatic protocol CT; however, MRI is also considered in some patients as a problem-solving tool [1]. Our study demonstrated that contrast-enhanced MRI almost has the same diagnostic performance for the detection of vascular involvement and for the determination of resectability as the pancreatic protocol CT. However, the evaluation tended to change from solid soft-tissue contact ≤180° or solid soft-tissue contact >180° on CT to no tumor contact or solid soft-tissue contact ≤180° on MRI. We believe that the major reason for this is the difference of section thickness between CT and MRI. Another reason was the presence of coronal reconstructed images in CT. Coronal images can easily visualize the relationship between primary tumor and the vascular which runs transversely across on the axial plane. We found no statistically significant difference in the resectability between CT and MRI in our study as well as vascular involvement. However, 7% (6/82, reviewer 1) and 12% (10/82, reviewer 2) of patients changed the resectability classification from borderline resectable to resectable. On the other hand, R0 resection rates were maintained even in MRI according to the findings from both reviewers (reviewer 1: 86%, 61/71) and (reviewer 2: 91%, 60/66). Recently, the NCCN guidelines mention the consideration of neoadjuvant therapy even in resectable disease. Therefore, even if MRI underestimates the resectability as “resectable”, which may be categorized as “borderline resectable” in CT, the treatment strategy is not going to make much difference irrespective of the initially used imaging modalities.Conclusion
Diagnostic performance in contrast-enhanced MRI for detecting vascular involvement and determining resectability of pancreatic ductal adenocarcinoma on the basis of the NCCN guideline were statistically comparable with CT. However, MRI can potentially underestimate the classification of the resectability.Acknowledgements
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.References
[1] NCCN clinical practice guidelines in oncology: pancreatic adenocarcinoma, version 2. 2021.Figures
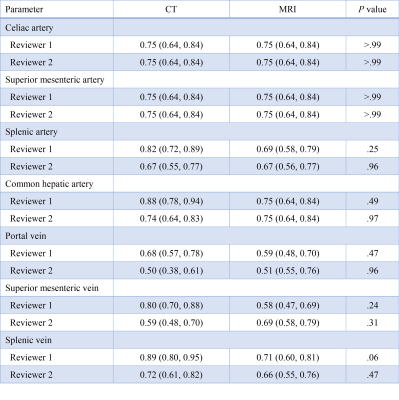
Table 1: Diagnostic Performance for
Vascular Involvement
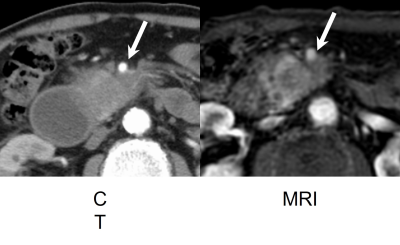
Figure 1. A 70-year-old
man with pancreatic ductal adenocarcinoma at body. Axial
contrast-enhanced (a)
MRI and (b) CT images show solid soft-tissue contact ≤ 180° to superior mesenteric artery (arrow) and diagnosed as
borderline resectable both on MRI and CT. Superior mesenteric arterial invasion
was pathologically confirmed.
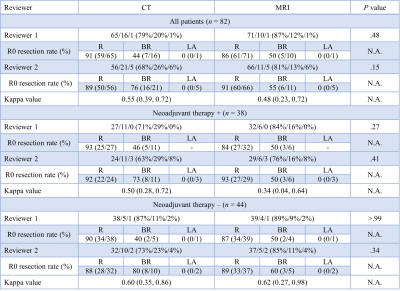
Table 2: Resectability and R0 Resection
Rate
DOI: https://doi.org/10.58530/2022/4230