4196
Image Quality of Deep-Learning Reconstructed Near-isotropic (3D) Enhanced MR enterography with LAVA HyperSense in Crohn disease patients1Radiology, Heaundae Paik Hospital, Busan, Korea, Republic of, 2GE Healthcare, Seoul, Korea, Republic of, 3GE Healthcare, Houston, TX, United States
Synopsis
In this study, we evaluate image quality of high resolution contrast-enhanced T1-weighted MR enterography with deep learning reconstruction. Use of DLRecon for near-isotropic CE-T1WI MRE provides improved image quality, and increased SNR.
Introduction
The contrast-enhanced T1-weighted (CE-T1W) coronal image is a key component of MR enterography (MRE) for Crohn’s disease (CD) evaluation (1). Due to bowel peristalsis or respiration and limited breath holding duration, it is challenging to obtain high resolution isotropic images without compromising image quality. Compressed sensing and deep learning reconstruction (DLRecon) enables near isotropic CE-T1W images with improved image quality during short scan time within one-breath hold. These 3D near-isotropic images allow high quality axial reformat images with identical contrast in same dynamic phase.In this study, we compared near-isotropic CE-T1W image of enteric phase with DLRecon (DLR), with conventional reconstruction and image filter (filtered) and with conventional reconstruction and no image filter (original) in terms of image quality.
Method
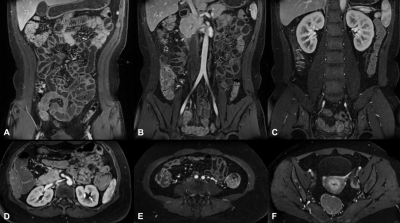
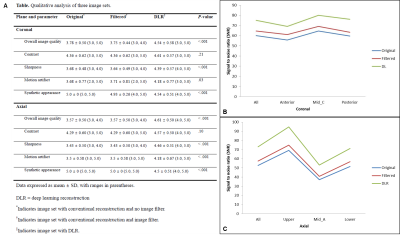
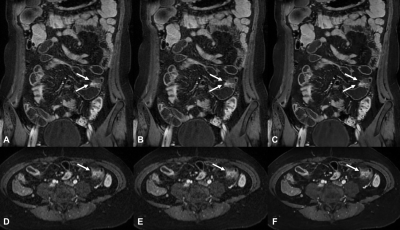
This retrospective study included 14 patients who underwent MRE for CD. Scans were acquired using a 3T MRI scanner (SIGNA™ Architect, GE Healthcare, Waukesha, USA), with two 30-channel surface coils (AIR™ anterior array coil). The coronal T1 weighted spoiled gradient-echo sequence (liver acquisition with acceleration volume acquisition; LAVA) with fat suppression was acquired during breathold, before contrast injection, and during enteric and portal phase, after intravenous (IV) administration of gadoterate meglumine (Dotarem, Guerbet, Aulnay-sous-Bois, France). The typical imaging parameters of the fat suppressed LAVA acquisition in the current study was as follows: voxel size = 1.3 x 1.5 x 1.6 mm, flip angle = 10, number of excitation = 1, bandwidth = 83.33 kHz. The scan time was approximately 17 seconds, varying slightly to accommodate the size of the patient. Three image sets of enteric phases were generated: one with conventional reconstruction and no image filter, one with conventional reconstruction and image filter (B – High sharpening, some smoothing), and one with deep learning reconstruction (DLRecon). These images sets were then reformatted into axial plane (slice thickness 1.4 mm). A 2D DLRecon algorithm (AIR Recon DL) (2), with denoising and sharpening properties, was retrained for 3D reconstruction, and was used for DLRecon. The network offered tunable noise reduction levels (25, 50 and 75%; higher levels indicated higher levels of denoising) and a factor of 75% was chosen for this study.Two radiologists independently assessed coronal and reformatted axial images of three enteric image sets (original, filtered, DLR) for subjective image quality using 5-point Likert scale (5=highest quality). Images were evaluated for overall image quality, contrast, sharpness and presence of motion artifact and synthetic appearance. For quantitative analysis, three representative locations were chosen on the coronal and axial planes, respectively (Figure 1). Signal to noise levels (SNR) were calculated by dividing the mean signal of the slice by the estimated standard deviation of noise. The noise levels were estimated by a hybrid Discrete Wavelet Transform (DWT) and edge information removal based algorithm which is described in detail, elsewhere (3).
Results
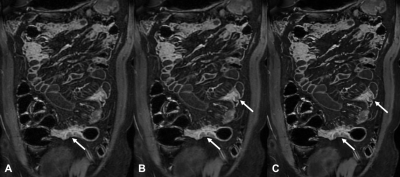
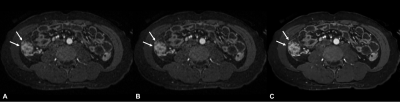
Both coronal and reformatted axial DLR images were significantly better than filtered and original images in overall image quality (4.54 ± 0.58 and 4.61 ± 0.50 for DLR, 3.75 ± 0.44 and 3.57 ± 0.50 for filtered, 3.78 ± 0.50 and 3.57 ± 0.50 for original; P < .001), sharpness (4.39 ± 0.57 and 4.46 ± 0.51 for DLR, 3.64 ± 0.49 and 3.43 ± 0.50 for filtered, 3.68 ± 0.48 and 3.43 ± 0.50 for original; P < .001), and motion artifact (4.18 ± 0.77 and 4.18 ± 0.67 for DLR, 3.71 ± 0.81 and 3.5 ± 0.58 for filtered, 3.68 ± 0.77 and 3.5 ± 0.58 for original; P=0.034 for coronal and P < .001 for axial). DLR image showed a significantly more synthetic appearance than filtered or original image. Contrast was not significant different between three image sets. DLR images showed the highest SNR in all location from both coronal and axial planes, followed by filtered and original images (P ≤ .001).Discussion
Our results showed that DLRecon significantly increased SNR and improved overall image quality, sharpness and decreases perception of motion artifact. Use of DLRecon enables high resolution near-isotropic CE-T1W MRE with sufficient image quality. It allows high quality axial reformatted image to be obtained from same dynamic phase, which is helpful for depicting anatomic details of bowel segment or extraluminal complication such as fistula or abscess (Figure 5).Conclusion
Use of DLRecon for near-isotropic CE-T1WI MRE provides improved image quality, and increased SNR.Acknowledgements
No acknowledgement found.References
1. Grand DJ, Guglielmo FF, Al-Hawary MM. MR enterography in Crohn’s disease: current consensus on optimal imaging technique and future advances from the SAR Crohn’s disease-focused panel. Abdom Imaging 2015;40:953-964.
2. Lebel RM. Performance characterization of a novel deep learning-based MR image reconstruction pipeline; arXiv preprint arXiv:200806559. 2020
3. Pimpalkhute, VA, Page R, Kothari A, Bhurchandi KM, Kamble VM. Digital Image Noise Estimation Using DWT Coefficients. IEEE Transactions on Image Processing 2021;30:1962-1972.
Figures