4183
Liver DWI using deep learning constrained compressed sensing: A primary study compared to conventional DWI and compressed sensing-based DWI
Ting Duan1, Zhen Zhang2, Hanyu Jiang2, Yidi Chen2, Xiaoyong Zhang3, and Bin Song2
1Radiology, West China Hospital, Sichuan University, Chengdu, China, 2West China Hospital, Sichuan University, Chengdu, China, 3Clinical Science, Philips Healthcare, Chengdu, China, Chengdu, China
1Radiology, West China Hospital, Sichuan University, Chengdu, China, 2West China Hospital, Sichuan University, Chengdu, China, 3Clinical Science, Philips Healthcare, Chengdu, China, Chengdu, China
Synopsis
Compressed sensing AI-based DWI substantially reduced noise artifacts and improved the signal-to-noise ratio and lesion contrast-to-noise ratio compared with conventional DWI and Compressed sensing based DWI, without any penalty for scan parameters. This technique may prove of value in better diagnostic liver imaging.
INTRODUCTION
Diffusion-weighted imaging (DWI) is an essential MRI sequence in liver imaging. Single-shot echo-planar imaging (SS-EPI) is widely used in liver diffusion studies given relatively short scanning time in insensitivity to physiologic motion. However, low signal-to-noise ratio (SNR), significant artifact, and geometric distortion are major disadvantages of EPI-DWI. In contrast, DWI with echo planar imaging (EPI) using compressed sensing reconstruction (EPI-CS-DWI) have been reported as a promising technique to overcome some limitations of EPI-DWI. However, one limitation will arise when diffusion imaging is conducted using large acceleration factors due to insufficient noise removal with CS. Recently, integrating artificial intelligence (AI) into the compressed sensing reconstruction has attracted much attention to further accelerate scans and improve image quality from highly undersampled k-space data[1]. Therefore, we aimed to evaluate the feasibility, image quality, and apparent diffusion coefficient (ADC) values of liver DWI using EPI with CS-AI (EPI-CS-AI-DWI) and to compare them with EPI-CS-DWI and conventional single-shot EPI (EPI-DWI).METHODS
This study was approved by the institutional ethics committee and written informed consent was obtained from all subjects. From September 2021 to October 2021, consecutive patients with focal liver lesions underwent liver MRI examinations on a 3T MRI scanner with a dedicated 32-channel phased-array breast coil (Ingenia Elition X, Philips Healthcare). DWI was obtained using free-breathing fat-suppressed conventional EPI-DWI, EPI-CS-DWI and EPI-CS-AI-DWI (with b-values of 0, 50 and 1000 s/mm2) in addition to the standard liver MRI protocol. The details of imaging parameters of EPI-DWI, EPI-CS-DWI and WPI-AI-CS DWI were as follows: FOV = 304×380mm2, TR/TE = 1665/56 ms, slice thickness= 6 mm, imaging matrix = 152×155, acceleration factor of both EPI-CS-DWI and EPI-CS-AI-DWI is 2.5.Quality of MR images was independently assessed by two radiologists (with 6 and 5 years of experience in liver MR imaging, respectively) using a 5-point Likert scale (1 = poor, 5 = excellent) in terms of sharpness of liver edge and vessel contour at liver hilum, image quality of the liver dome, severity of artifacts, overall image quality and lesion conspicuity. For quantitative assessment, using the method similar to Xie et al [2], representative region of interest was carefully drawn on the slice with the largest cross section of the lesion and liver on the b = 1000 s/mm2 images and corresponding ADC maps of EPI-DWI, EPI-CS-DWI and EPI-CS-AI-DWI respectively. SNR, lesion contrast-to-noise ratio (CNR) were also calculated for comparison. Inter-observer agreement was assessed using Cohen’s kappa efficiency for subjective and objective assessments. The Likert scales and quantitative parameters were compared using the Wilcoxon signed-rank test. If significant, Bonferroni posthoc test was performed for pairwise comparisons. A p value less than 0.05 was considered significant.RESULTS
A total of 29 patients (mean age, 63.25; 24 men) were included during the study period. The image quality scores and ĸ values for sharpness of liver edge and vessel contour at liver hilum, image quality of the liver dome, severity of artifacts, overall image quality and lesion conspicuity of EPI-DWI, EPI-CS-DWI and EPI-CS-AI-DWI are summarized in Table 1. Mean image scores for the sharpness of liver edge and vessel contour at liver hilum, liver dome, severity of artifacts and overall image quality were significantly higher in EPI-CS-AI-DWI compared with EPI-DWI and EPI-CS DWI (P < 0.05 for all; Figure 1 and 2). EPI-CS-AI-DWI also demonstrated the best lesion conspicuity, however the difference was not statistically significant. Among the three techniques, the highest SNR and CNR were obtained with EPI-CS-AI-DWI, (Table 2), followed by EPI-CS DWI. The ĸ values ranged from 0.35 to 0.79, indicating moderate to good agreement between the two reviewers.DISCUSSION and CONCLUSION
This study demonstrated that EPI-CS-AI-DWI could improve image quality and reduce artifact of liver compared with EPI-CS-DWI and EPI-DWI in aggressive setting using SENSE and CS factors of 2.5. The mean SNR values of the liver and lesion were significantly higher in EPI-CS-AI-DWI compared with the other two approaches. AI would enable it possible to select aggressive acceleration factor as an option for higher image quality in DWI without any penalty for scan parameters. DWI is important for focal liver lesion detection and characterization. However, disadvantages of DWI are low SNR and influenced by motion artifacts. Some reconstruction methods, such as EPI combined with CS, have been introduced in clinical MRI. However, the image quality at high acceleration factors can be degraded by noise amplification and/or undersampling artifacts[3]. moreover, it is challenging with CS in finding an appropriate sparse transform for specific applications and manually tuning the hyperparameters, which is a time-consuming process that is difficult to standardize[4]. Recent progress in AI opens a new possibility to solve the inverse problem of MR image reconstruction in an efficient manner. Sheng et al[5] suggested that AI-based reconstruction method has preponderance in noise suppression, structural preservation and lesion detection on T2WI in liver. Our results further proved the superiority of AI-based reconstruction method in liver DWI, and verified that EPI-CS-DWI with AI-based reconstruction significantly reduced motion artifacts and image noise at the same time.Acknowledgements
NoneReferences
1 Tajima T, Akai H, Sugawara H, Yasaka K, Kunimatsu A, Yoshioka N, Akahane M, Ohtomo K, Abe O, Kiryu S. Breath-hold 3D magnetic resonance cholangiopancreatography at 1.5 T using a deep learning-based noise-reduction approach: Comparison with the conventional respiratory-triggered technique. Eur J Radiol 2021; 144: 109994 [PMID: 34627106 DOI: 10.1016/j.ejrad.2021.109994] 2 Xie SM, Masokano IB, Liu WG, Long XY, Li GJ, Pei YG, Li WZ. Comparing the clinical utility of single-shot echo-planar imaging and readout-segmented echo-planar imaging in diffusion-weighted imaging of the liver at 3 tesla. European Journal of Radiology 2021; 135 [PMID: WOS:000614698000013 DOI: ARTN 109472 10.1016/j.ejrad.2020.109472] 3 Taouli B, Sandberg A, Stemmer A, Parikh T, Wong S, Xu J, Lee VS. Diffusion-weighted imaging of the liver: comparison of navigator triggered and breathhold acquisitions. J Magn Reson Imaging 2009; 30(3): 561-568 [PMID: 19711402 DOI: 10.1002/jmri.21876] 4 Kaga T, Noda Y, Mori T, Kawai N, Takano H, Kajita K, Yoneyama M, Akamine Y, Kato H, Hyodo F, Matsuo M. Diffusion-weighted imaging of the abdomen using echo planar imaging with compressed SENSE: Feasibility, image quality, and ADC value evaluation. Eur J Radiol 2021; 142: 109889 [PMID: 34388627 DOI: 10.1016/j.ejrad.2021.109889] 5 Sheng RF, Zheng LY, Jin KP, Sun W, Liao S, Zeng MS, Dai YM. Single-breath-hold T2WI liver MRI with deep learning-based reconstruction: A clinical feasibility study in comparison to conventional multi-breath-hold T2WI liver MRI. Magn Reson Imaging 2021; 81: 75-81 [PMID: 34147594 DOI: 10.1016/j.mri.2021.06.014]Figures
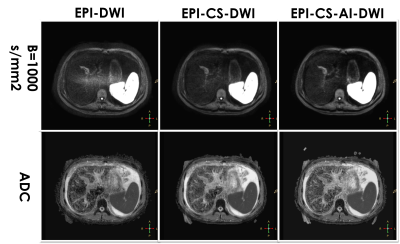
EPI-DWI, EPI-CS-DWI and EPI-CS-AI-DWI images (b = 1000 s/mm2) and corresponding ADC maps of a 56-year-old male patient with hepatocellular carcinoma at the level of liver hilum. Noise-like artifacts are detected at the center of the EPI-DWI image and corresponding ADC map. These artifacts are reduced on EPI-CS-DWI, EPI-CS-AI-DWI, and corresponding ADC maps. EPI-CS-AI-DWI has the best image quality and improved the depiction of portal vein contour among three techniques.
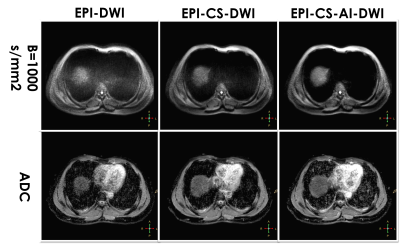
EPI-DWI, EPI-CS-DWI and EPI-CS-AI-DWI images (b = 1000 s/mm2) and corresponding ADC maps of a 50-year-old male patient with hepatocellular carcinoma at the level of liver dome. Transversal noise-like artifacts are detected at the center of the EPI-DWI image and ADC map, but are reduced on EPI-CS-DWI, EPI-CS-AI-DWI, and corresponding ADC maps. EPI-CS-AI-DWI has the best image quality among three techniques.
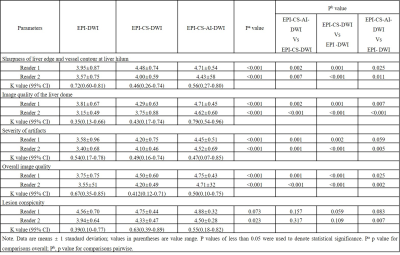
Table 1 The image quality
scores for sharpness of liver edge and vessel contour at liver hilum, image
quality of the liver dome, severity of artifacts, overall image quality and
lesion conspicuity.
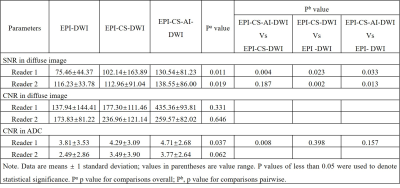
Table 2 SNR and CNR for diffuse
image (b=1000 2 ) and CNR for ADC
DOI: https://doi.org/10.58530/2022/4183