4177
Time estimation from stroke onset with diffusion-relaxation matrix-based T2 and ADC simultaneous mapping
Hajime Yokota1, Takayuki Sakai2, Masami Yoneyama3, and Takashi Uno1
1Department of Diagnostic Radiology and Radiation Oncology, Chiba University, Chiba, Japan, 2Department of Radiology, Eastern Chiba Medical Center, Togane, Japan, 3Philips Japan, Tokyo, Japan
1Department of Diagnostic Radiology and Radiation Oncology, Chiba University, Chiba, Japan, 2Department of Radiology, Eastern Chiba Medical Center, Togane, Japan, 3Philips Japan, Tokyo, Japan
Synopsis
Diffusion-relaxation matrix (DRM) sequence consists of dual-echo single-shot DW-EPI. DRM was able to detect acute cerebral infarction as well as conventional DWI, and can simultaneously acquire ADC and T2 values. T2 values in the infarcted area correlated significantly with time since stroke onset, whereas ADC did not. In addition, T2 values could predict whether the infarct was within 4.5, 6, or 16 hours, which are the thresholds for thrombolysis and endovascular treatment.
Introduction
Estimating the time from onset is essential to determine the treatment strategy for stroke. However, accurate onset time cannot be estimated in the case of wake-up stroke or when there are no bystanders.[1] Although apparent diffusion coefficient (ADC) is essential for the diagnosis of acute infarction, it is not useful for the estimation of onset time in the hyperacute to acute phase. Infarcts in these phases only show low ADC values. T2 value is a widely used quantitative marker that has been reported to correlate with infarct onset time. However, additional imaging is required to measure the T2 value. In this study, we evaluated an imaging method called diffusion-relaxation matrix (DRM), which can simultaneously collect ADC and T2 maps by dual-echo single-shot diffusion-weighted echo-planar imaging (DW-EPI).Materials and methods
SubjectsThe consecutive patients considered acute ischemic stroke were prospectively involved in this study. All subjects were examined with a 1.5T whole-body clinical system (Ingenia, Philips Healthcare). Stroke protocol included FLAIR, diffusion-weighted image (DWI) (b = 0 and 1000, TE = 64 ms, TR = 7720 ms, field of view = 230 x 230 mm, matrix = 112 x 156, thickness = 5 mm, scan duration = 1 min 3 sec), MR angiography. When the bystander radiologist detected acute stroke on diffusion-weighted image, DRM (Figure 1) (b = 0 and 1000, TE = 48 and 120 ms, TR = 3000 ms, field of view = 250 x 234, matrix = 124 x 164, thickness = 5 mm, scan duration = 2 min 42 sec) was added in the stroke protocol. Patients with a clear onset time were included in the analysis. The time from onset to MRI was collected from the medical record.
Visual assessment
We checked whether the lesions that showed high signals on conventional DWI also showed high signals on DWI derived from DRM (short echo, b = 1000).
Quantitative analysis
The T2 and ADC maps were created with in-house software. Two ADC maps were output from short and long echo images, while two T2 maps were output together from b = 0 and b = 1000 images. A circular region of interest (ROI) was placed in the region of high signal in the diffusion-weighted image (short echo, b=1000) to avoid the partial volume effect (Figure 2). The mean ADC and T2 values in the ROI were used for further analysis. The ratio of infarct to the contralateral normal area was calculated.
Statistics
The correlations between onset time vs. ADC and T2 values were evaluated by Spearman's rank correlation. Receiver operating characteristic (ROC) analysis was performed to calculate the area under the curve (AUC) whether the onset was within 4.5, 6, or 16 hours.
Results
Forty-five patients underwent MRI, including DRM, and 18 of the 45 patients presented a clear onset time. Eighteen patients (78.6±8.6 years; 16 men and 9 women; cerebral artery area 11, pons 3, thalamus 3, cerebellum 1) had 25 MRIs including DRM and were included in the following analyses. T2 values of the infarcted area were significantly correlated to the time from onset in both short and long echo images by Spearman's rank correlation test. The scatter plot of the time and T2 values is shown in Figure 3. The ratio of the infarcted area to the contralateral normal area also showed a significant correlation. The AUCs for these values were 0.800 or higher for estimating the time within 4.5, 6, and 16 hours. As for within 4.5 and 6 hours, the T2 value of the infarcted area (b = 1000) had the highest AUC, 0.971. The list of AUCs and ROC curves is shown in Figures 4 and 5. The AUC for whether the onset was within 16 hours or not had the highest ratio to the contralateral side, 0.904 for both b = 0 and b = 1000 images.Discussion
MRI is expected to be used as a biomarker to estimate stroke onset because infarction changes dynamically by sequences such as DWI and FLAIR. Although DWI-FLAIR mismatch is widely used to predict infarction within 4.5 hours, its low sensitivity is a problem.[2] Although there are several papers that focus on T2 values, they use multi-echo T2 mapping or synthetic MRI, which needs an additional sequence.[3,4] DRM is a sequence that can simultaneously diagnose acute ischemic stroke and estimate onset time in a short scan time.Within 4.5 hours of onset, transvenous thrombolysis is indicated.[5] Although the indications for endovascular treatments are gradually expanding, 6 and 16 hours are the widely used thresholds. T2 mapping using DRM correlated with onset time and allowed us to estimate these time thresholds with high accuracy. Although there have been studies that predicted the onset time within 4.5 hours, studies that examined the onset time within 6 or 16 hours have been rare.
Conclusion
DRM is a sequence that can detect acute infarction and estimate onset time in a short scan time. T2 values obtained from DRM correlate with onset time and can determine with high accuracy whether treatment is indicated or not.Acknowledgements
No acknowledgement found.References
- Mackey J, Kleindorfer D, Sucharew H, Moomaw CJ, Kissela BM, Alwell K, Flaherty ML, Woo D, Khatri P, Adeoye O, Ferioli S, Khoury JC, Hornung R, Broderick JP. Population-based study of wake-up strokes. Neurology 2011;76:1662–1667. doi: 10.1212/WNL.0b013e318219fb30.
- Thomalla G, Cheng B, Ebinger M, Hao Q, Tourdias T, Wu O, Kim JS, Breuer L, Singer OC, Warach S, Christensen S, Treszl A, Forkert ND, Galinovic I, Rosenkranz M, Engelhorn T, Köhrmann M, Endres M, Kang D-W, Dousset V, Sorensen AG, Liebeskind DS, Fiebach JB, Fiehler J, Gerloff C, STIR and VISTA Imaging Investigators. DWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4·5 h of symptom onset (PRE-FLAIR): a multicentre observational study. Lancet Neurol 2011;10:978–986. doi: 10.1016/S1474-4422(11)70192-2.
- Duchaussoy T, Budzik J-F, Norberciak L, Colas L, Pasquini M, Verclytte S. Synthetic T2 mapping is correlated with time from stroke onset: a future tool in wake-up stroke management? Eur Radiol 2019;29:7019–7026. doi: 10.1007/s00330-019-06270-0.
- Siemonsen S, Mouridsen K, Holst B, Ries T, Finsterbusch J, Thomalla G, Ostergaard L, Fiehler J. Quantitative t2 values predict time from symptom onset in acute stroke patients. Stroke 2009;40:1612–1616. doi: 10.1161/STROKEAHA.108.542548.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL, American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018;49:e46–e110. doi: 10.1161/STR.0000000000000158.
Figures

Sequence diagram of diffusion-relaxation matrix (DRM) sequence consists of dual-echo single-shot DW-EPI without prolongation of acquisition time. DRM produces four images, a combination of b = 0 and 1000, short and long echo time.
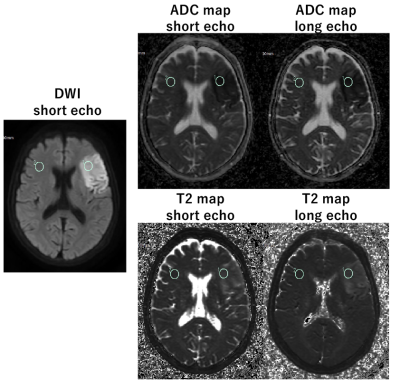
Acute cerebral infarction in the left middle cerebral artery perfusion zone. ROIs were set in the infarcted area and the contralateral normal area. The mean value of this region was obtained from two ADC maps and two T2 maps. The ratio of the infarcted area to the normal area was also calculated.

Spearman's rank correlation test showed significant correlations in T2 value and T2 ratio (*). In the ROC analysis, these values were possible to determine if the stroke onset was within 4.5, 6, or 16 hours with an AUC of 0.9 or greater.

Scatter plots of T2 value, T2 ratio, and time from onset of cerebral infarction, which had a significant correlation. T2 value showed a high correlation value for both short and long echo images.

ROC curves from onset within 4.5, 6, and 16 hours. Curves with high AUC values (bold in Fig. 3) are shown.
DOI: https://doi.org/10.58530/2022/4177