4175
Atherosclerotic ischemic recurrent stroke patients: a nomogram model of risk factors and risk prediction1Shaanxi Provincial People's Hospital, Xi’an, China, 2Philips healthcare, Xi’an, China
Synopsis
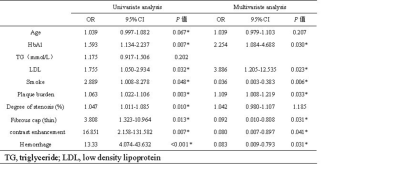
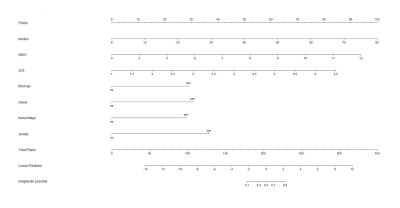
The aim of this study was to construct a diagnostic model of recurrent stroke with the combination of high resolution MRI imaging characteristics and clinical parameters. The vessel wall characteristics of plaque and clinical data were compared between stroke and recurrent stroke patients. Multivariate logistic regression analysis was explored, seven risk factors (plaque burden, fibrous cap, hyperdense, hemorrhage, HbA1, low density lipoprotein and smoke) were independent risk factors for recurrent stroke patients. Then a nomogram model was established for risk prediction.
Introduction
The incidence of stroke caused by atherosclerotic stenosis was 46.6%[1],the risk of recurrent stroke in the first year after stroke is estimated to be about 11% globally[2], Due to the high mortality and disability rates associated with recurrent stroke, early detection of recurrent stroke is important. Common risk factors for recurrent stroke include hypertension, diabetes, hyperlipidemia, obesity and so on[3]. Ischemic stroke occurs when a plaque ruptures, exposing the lipid core to flowing blood, causing a clot and block the distal artery branch. MRI is the emerging way to observe the biometrics of plaque features which has high resolution and contrast. In this study, we intended to provide clues for early identification and screening of high-risk patients with recurrent ischemic stroke by establishing a reliable and accurate rate risk prediction model.Methods
One hundred and ten patients with intracranial large artery atherosclerotic stroke were recruited. Then the patients were followed up and divided into the non-recurrent stroke group and the recurrent stroke group according to neuropsychiatric symptoms and imaging characteristics one year later. All MRI images were obtained by using a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands) with a 32 channel head coil. The scan sequences included conventional brain MRI (T1WI, T2WI, FLAIR, DWI, TOF-MRA) and high resolution MRI sequences (BB-T1WI, BB-T2WI, CE-T1WI, PD Vista). The differences of vessel wall properties of plaque (maximum wall thickness, vessel area, vessel fluid area and vessel wall area of narrowest level, plaque burden, degree of stenosis, remodeling index, fibrous cap, contrast enhancement, hemorrage) and clinically relevant factors (smoking, hypertension, HbA1, hyperlipidemia, hyperhomocysteinemia) of the two groups were analyzed. Continuity values in this study were expressed as (`x±s), and count data were expressed as frequency (percentage). Quantitative data were compared using independent sample t test or Mann-Whitney U test, and χ2 test was used for counting data. The risk factors were analyzed by univariate and multivariate logistic regression. Univariate analysis with statistical significance (P < 0.05) were included in multivariate logistic regression analysis. After screening for independent risk factors using the logistic regression model, the nomograms were drawn using the R 3.5.3 software package, and a nomogram prediction model was established using the RMS package. ROC and RMS program packages were used for receiver operating characteristic (ROC) curve analysis. The consistency index (C-index) calculated by RMS program package represents the ROC curve prediction accuracy, the value range of C-index was 0. 5 ~ 1. 0.Results
Nineteen people (14 men; 59.26±16.50years) were in the recurrent stroke group , 91 people (69 men, 52.87±12.78 years) were in the stroke group. There was significant difference between the two groups in age, HbA1, TG, LDL, smoke, plaque burden, degree of stenosis, thin fibrous cap, contrast enhancement and hemorrhage (table 1); Univariate analysis showed that the statistically significant risk factors were age, HbA1, LDL, smoke, plaque burden, degree of stenosis, thin fibrous cap, contrast enhancement and hemorrhage. The seven factors (HbA1, LDL, smoke, plaque burden, thin fibrous cap, contrast enhancement and hemorrhage) were independent risk factors of recurrent patients (table 2). We conducted collinearity diagnostics for the above independent risk factors, and the variance inflation factors (VIFs) were 1.151, 1.093, 1.018, 1.172, 1.108, 1.087 and 1.170 respectively, suggesting that there was no multiple collinearities among the seven independent risk factors. Based on the logistic multivariate regression analysis, the seven independent risk factors were included in the prediction model, then an individualized nomogram prediction model of recurrent stroke was established (figure 1). The AUC value of recurrent stroke in stroke patients is 0.957 [95% confidence interval (CI); 0.789–0.978], suggesting that the nomogram prediction model has an excellent discrimination (figure 2).Discussion
We concluded that there were significant differences in plaque characteristics (plaque burden, thin fibrous cap, contrast enhancement and hemorrhage) and clinical factors (HbA1, LDL and smoke) between two groups. Hyperglycemia can lead to thickening of vascular basement membrane, increase of new blood vessels, decreased differentiation, proliferation, adhesion of endothelial progenitor cells, weakened plaque repair ability, break the balance between plaque rupture and plaque healing and resulting in the occurrence of stroke[4, 5]. Passive smoking can lead to atherosclerosis, and the levels of low-density lipoprotein cholesterol can also be elevated by smoking[6]. Ran et al.[7] showed that plaque burden can predict not only stroke occurrence but also stroke recurrence, large plaque load tends to have significant lumen stenosis rate and large plaque surface tension, leading to plaque rupture and hypoperfusion of responsible vessel distribution area, inducing ischemic stroke. The thin fibrous cap makes the plaque surface more prone to rupture upon receiving hemodynamic changes. The enhancement of plaques is closely related to the destruction of intracranial blood brain barrier. Combined with the above mentioned risk factors, we can better predict the recurrence of stroke.Conclusion
In this study, we demonstrated the vessel wall characteristics of plaque and clinical data usefulness of the diagnostic models, through the combination of plaque burden, fibrous cap, contrast enhancement, hemorrage, and clinical parameters including HbA1, LDL, smoke, we could predict the probability of recurrent stroke in patients who have already had stroke, which helps to improve the early identification and screening of such high-risk patients.Acknowledgements
noReferences
[1]. Wang, Y., et al., Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke, 2014. 45(3): p. 663-9. [2]. Mohan, K.M., et al., Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke, 2011. 42(5): p. 1489-94.[3]. Singh, R.J., et al., Long-term neurological, vascular, and mortality outcomes after stroke. Int J Stroke, 2018. 13(8): p. 787-796. [4]. Vergallo, R. and F. Crea, Atherosclerotic Plaque Healing. N Engl J Med, 2020. 383(9): p. 846-857. [5]. Yu, X., et al., Blood Brain Barrier Disruption in Diabetic Stroke Related to Unfavorable Outcome. Cerebrovasc Dis, 2016. 42(1-2): p. 49-56. [6]. Aune, D., et al., Tobacco smoking and the risk of sudden cardiac death: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol, 2018. 33(6): p. 509-521. [7]. Ran, Y., et al., Higher Plaque Burden of Middle Cerebral Artery Is Associated With Recurrent Ischemic Stroke: A Quantitative Magnetic Resonance Imaging Study. Stroke, 2020. 51(2): p. 659-662.
Figures