4165
Predictive value of cardiac magnetic resonance for reverse left ventricular remodeling after acute ST-segment elevation myocardial infarction1Department of Radiology, the First Medical center, Chinese People's Liberation Army Hospital, Beijing, China., Beijing, China, 2Philips Healthcare, Beijing, China, Beijing, China
Synopsis
Many ST-segment elevation myocardial infarction (STEMI) patients treated with primary percutaneous coronary intervention (PCI) are still exposed to a consequence known as left ventricular (LV) remodeling. Most studies have reported that reverse LV remodeling is associated with improved patient outcomes. Cardiac magnetic resonance (CMR) imaging has become a beneficial imaging modality to assess myocardial morphology, LV function and infarct characteristics simultaneously. This study assesses the predictive role of LV volume, LV function and infarct characteristics by CMR on reverse LV remodeling after STEMI. Our data showed that peak CK-MB, extent of MVO volume of LV were independent predictors of reverse LV remodeling.
Introduction
Many ST-segment elevation myocardial infarction (STEMI) patients treated with primary percutaneous coronary intervention (PCI) are still exposed to a chronic consequence of myocardial infarction (MI) known as left ventricular (LV) remodeling. From a practical perspective, the pattern of remodeling can be categorized into two groups: that reverse LV remodeling which achieves functional recovery and adverse LV remodeling that which is irreversible.1 Most clinical studies have reported that reverse LV remodeling is associated with an improvement in patient outcome.2,3 Cardiac magnetic resonance (CMR) imaging has progressively evolved to become an indispensable tool in cardiology. Compared to speckle tracking echocardiography (STE), CMR imaging measures the left ventricle (LV) providing unique insight for the process of myocardial injury. Cardiac magnetic resonance feature tracking (CMR-FT) is a new post-processing technique that provides myocardial strain parameters, with the advantages of not requiring additional sequences and a relatively short post-processing time.4 So far, there was few studies specifically designed to address reverse LV remodeling after STEMI at CMR. The aim of this study was to assess the predictive role of LV volume, LV function and infarct characteristics by CMR on reverse LV remodeling after STEMI.Materials and Methods
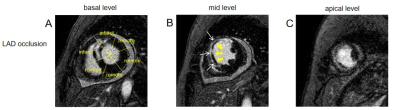
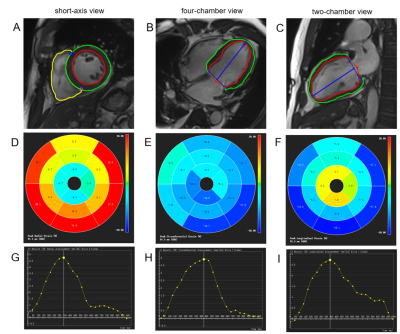
Eighty six STEMI patients were included in this study: 37 subjects with reverse LV remodeling (33 males; mean age±standard deviation: 56±10 years), 49 subjects with no reverse LV remodeling (43 males; 55±13 years). Reverse LV remodeling following STEMI has been defined as ≥10% decrease in LV end-systolic volume (LVESV) from baseline. The patients were scanned using 1.5 T scanner (Multiva, Philips Medical Systems, Netherlands) 5-day and 5-month after successful percutaneous coronary intervention (PCI) treatment. Cardiac function was evaluated by balanced turbo field echo (BTFE) cine sequence at the continuous short-axis covering the whole left ventricle (LV) and the long-axis (2/3/4 chamber) views under breath-holding. Imaging parameters included TR/TE 3.7/1.8ms, in-plane resolution 1.4 × 1.4mm2, flip angle 60° and slice thickness 8mm with 8 to 12 slices gathered on the short-axis. Late gadolinium enhancement (LGE) imaging was performed 10 to 15 minutes after administration of 0.2mmol/kg gadolinium-based contrast agent (Gadopentetate Dimeglumine, BeiLu, Beijing, China) using a segmented phase-sensitive inversion-recovery fast gradient-echo pulse sequence (PSIR). The slice location was consistent with the cine sequence. Other imaging parameters included TR/TE 6.2/3ms, in-plane resolution 1.6×1.65mm2, flip angle 25° and slice thickness 8mm. All CMR parameters of LV volume and function were retrospectively analyzed using dedicated software (cvi42 v5.3, Circle Cardiovascular Imaging, Calgary, Canada), which was completed by experienced operators without knowledge of the clinical data. LV volumes and functional parameters were derived from the analysis of cine sequences, which included parameters such as including end-diastolic volume (EDV), end-diastolic volume/body surface area (EDV/BSA), end-systolic volume, ESV/BSA, Stroke volume (SV), SV/BSA, LVEF, cardiac output (CO), and cardiac index (CI). Infarct characteristics were assessed by analyzing Late gadolinium enhancement (LGE) sequences. The LV myocardium is divided into the infarct zone and the remote zone (Figure 1). Microvascular obstruction (MVO) was defined on the LGE images as hypointense area within the hyper enhanced myocardium (Figure 1). MVO area was included in the infarct area. Global and regional strains and associated strain rates, as well as displacements and associated velocities in radial, circumferential and longitudinal directions were assessed by CMR-FT from cine images using feature-tracking post-processing method. Firstly, the epicardial and endocardial contours of the LV myocardium in end-systolic and end-diastolic phases were traced. Epicardial and endocardial borders were automatically propagated to the other phases by the software. Then, the strain in radial, circumferential and longitudinal directions was recorded at global and segmental levels and plotted against time (Figure 2). Logistic regression was used to identify factors associated with adverse LV remodeling.Results
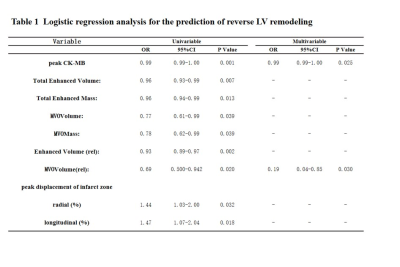
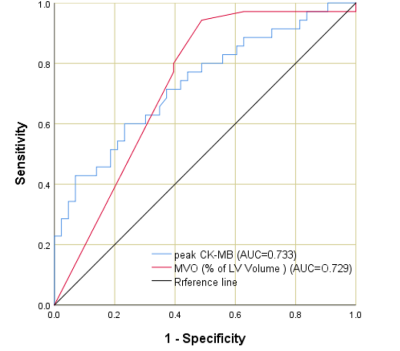
In univariable logistic regression analysis, peak creatinine kinase isoenzyme (CK-MB), total enhanced volume and mass, MVO volume and mass, extent of enhanced and MVO volume of LV, the peak displacement of infarct zone in radial and longitudinal directions showed significant predictive associations with the reverse LV remodeling (Table 1, p <0.05). Multivariate logistic regression with the backward stepwise method was used to identify the predictors of reverse LV remodeling. The variables with p < 0.05 in univariate analysis were included in the multivariable model. In multivariable logistic regression analysis, peak CK-MB (Table 1, odds ratio: 0.99[0.99–1.00], p=0.025), extent of MVO volume of LV (Table 1, odds ratio: 0.19[0.04–0.85], p=0.030) were independent predictors of reverse LV remodeling. In the ROC analyses, the predictive value of peak CK-MB (AUC = 0.733, 95% CI = 0.621–0.845 p < 0.001) and extent of MVO volume of LV (AUC = 0.729, 95% CI = 0.615–0.842 p = 0.001)was similarly good(Figure 3).Conclusions
The main findings of the present study were as follows: (a) In this study, CMR showed reversal of LV remodelling in 43% of patients with STEMI and (b) peak CK-MB, extent of MVO volume of LV were independent predictors of reverse LV remodeling.Acknowledgements
No acknowledgement foundReferences
References
1 Park YH, Kang SJ, Song JK ,et al. Prognostic value of longitudinal strain after primary reperfusion therapy in patients with anterior-wall acute myocardial infarction. J Am Soc Echocardiogr 2008;21:262–267.
2 Breithardt OA. Reversing heart failure by CRT: how long do the effects last? Eur Heart J 2013;34:2582–2584.
3 Linde C, Gold MR, Abraham WT, et al. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction (REVERSE) study. Eur Heart J 2013;34:2592–2599.
4 Schuster A, Hor KN, Kowallick JT, Beerbaum P, Kutty S.Cardiovascular magnetic resonance myocardial feature tracking: concepts and clinical applications. Circ Cardiovasc Imaging 2016;9:e004077.
Figures