4164
Left ventricular diastolic dysfunction in uncomplicated obesity: evaluated by CMR tissue tracking and volume-time curve1Radiology, West China Hospital, Sichuan University, Chengdu, China, 2Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, China, 3MR Collaboration, Siemens Healthineers Ltd., Shanghai, China
Synopsis
This study evaluated left ventricular (LV) diastolic functional changes and left atrial (LA) functional indices using cardiac magnetic resonance (CMR) tissue tracking and volume-time curve in obese adults with no clinical signs or comorbidities. The association of LV diastolic function with fat distributions was also assessed. The results showed that CMR detected subclinical LV diastolic dysfunction, impaired LA reservoir and conduit function with preserved LV ejection fractions in adults with obesity. LV diastolic function was associated with LA reservoir and conduit function. Visceral fat was deleterious for LV diastolic function, while peripheral obesity might have had a protective effect.
Introduction
Obesity has become an epidemic in China since the beginning of the 21st century, with an estimated 0.32% per year increase in prevalence1. Obesity-related comorbidities, such as diabetes, hypertension, and coronary heart disease, are major risk factors contributing to heart failure. However, in obese individuals with no clinically apparent cardiovascular risk factors, subclinical structural and functional changes have also been identified2, which predisposes these individuals to an increased risk of heart failure. The early effects of uncomplicated obesity on left ventricular (LV) diastolic dysfunction combined with left atrial (LA) function have not been well clarified. In addition, previous studies have found that different regions of fat deposition have varied effects on the heart. However, the method of measuring body fat distributions has not been unified. Dual X-ray absorptiometry (DXA) has also been extensively applied as it allows accurate regional fat distribution assessments, including android, trunk, gynoid, upper and lower extremity, and visceral fat. We aimed to assess LV diastolic dysfunction and LA function using cardiac magnetic resonance (CMR) tissue tracking and volume-time curves in adults with uncomplicated obesity. We also evaluated the association of these measurements with fat distributions.Methods
We prospectively enrolled 40 obese participants (BMI≥ 27.5 kg/m2) and 30 healthy controls (18.5 ≤ BMI ≤ 23.5 kg/m2) between 18 and 60 years old who underwent CMR on a 3T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). BMI was categorized into the following three groups: healthy weight (18.5-23.0 kg/m2), overweight (23.0-27.5kg/m2), and obesity (≥27.5kg/m2)3. Subjects were excluded if they had any of the following conditions: hypertension or diabetes measured with oral glucose tolerance; history of cardiovascular diseases or any cardiovascular procedures; major systemic diseases that could affect the myocardium, such as connective tissue diseases and sarcoidosis; endocrine disease, such as hyperthyroidism and hypothyroidism; metabolic diseases, such as a history of alcohol abuse or amyloidosis; obstructive sleep apnea; any contraindication to CMR imaging; and poor image quality. A segmented breath-hold balanced steady-state free precession (bSSFP) sequence was used to obtain ventricular short-axis cine images and two- and four-chamber cine images in the long-axis view. The bSSFP parameters are as follows: TR/TE=3.3/1.22 ms, flip angle=41°, slice thickness=8 mm, field of view=360 × 320 mm2, matrix size=208 × 166, and a temporal resolution=39.34 ms. The LV functional parameters based on strain rate analysis (radial, circumferential, and longitudinal peak diastolic strain rates[PDSR], and peak systolic strain rates[PSSR]) and volume-time curve analyses (peak filling rate[PFR], peak ejection rate[PER], PER normalized to end‑diastolic volume[PER/EDV], and PFR normalized to EDV [PFR/EDV]), and LA functional indices (reservoir function: LA total ejection fraction [EF], total strain[εs], peak positive SR[SRs]; conduit function: LA passive EF, passive strain[εe], peak early negative SR[SRe]; and booster pump function: LA active EF, active strain[εa], peak late negative SR[SRa]) were compared between the two groups. Body fat distributions were measured with dual X-ray absorptiometry. Pearson correlations were used to analyze the associations between LV diastolic functional parameters and LA functional indices. Correlations among fat distributions and LV diastolic function indices were conducted with multivariable linear regression.Results
Compared with controls, obese participants had impaired LV diastolic function with lower circumferential and longitudinal peak diastolic strain rates (PDSR) and PFR/EDV (all p <0.05), while LV systolic function parameters (LVEF, PSSR in three directions and PER/EDV) were not significantly different between the two groups (p >0.05). LA reservoir function (SRs) and conduit function (passive EF, εe, and SRe) decreased, and booster pump function (εa and SRa) increased in the obese group compared with the control group (all p <0.05). LV diastolic functional parameters were moderately correlated with LA reservoir and conduit function, whereas they were not related to LA booster pump function. Multivariable linear regression controlling for age, sex, height, and systolic blood pressure showed that circumferential PDSR was positively correlated with lower extremity and gynoid fat, and hip circumference. Radial PDSR was positively correlated with lower extremity fat. PFR/EVD was positively correlated with gynoid fat. In contrast, visceral fat was inversely associated with longitudinal PDSR. In addition, LAEFs from the volumetric analysis had moderately strong correlations with corresponding longitudinal strain and strain rates; among these, LA passive EF had the strongest correlation with SRe (r = 0.657).Discussion and Conclusions
This study compared LV and LA functional parameters in obese adults with no clinical signs or comorbidities with normal controls. It also revealed that some of these changes were associated with fat distributions in the adults with obesity. We found that obesity is associated with impaired LV diastolic function and preserved systolic function. In addition, obese individuals have impaired LA reservoir and conduit function and higher booster function, which may be compensatory. LV diastolic function is associated with LA reservoir and conduit function, rather than booster pump function. Visceral fat has a deleterious effect on LV diastolic dysfunction, while peripheral obesity (lower extremity and gynoid fat distributions and hip circumference) might have a protective effect. These findings indicated that CMR tissue tracking, and volume-time curves can detect subclinical LV diastolic dysfunction with preserved LV ejection fractions in obese adults. Fat distributions have different effects on cardiac function and might contribute to obesity management in clinical practiceAcknowledgements
This work was supported by the National Natural Science Foundation of China [Grant number. 81601462], the Key Research & Development Project of Science and Technology of Sichuan Province (Grant number. 21ZDYF1602), 1.3.5. project for disciplines of excellence, West China Hospital, Sichuan University (Grant number. ZYGD18017).
References
1. Tian Y, Jiang C, Wang M, et al. BMI, leisure-time physical activity, and physical fitness in adults in China: results from a series of national surveys, 2000-14. Lancet Diabetes Endocrinol. 2016;4(6):487-497.
2. Orhan AL, Uslu N, Dayi SU, et al. Effects of isolated obesity on left and right ventricular function: a tissue Doppler and strain rate imaging study. Echocardiography. 2010;27(3):236-243.
3. Chen YJ, Peng Q, Yang Y, et al. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: a repeated cross-sectional study. Bmc Public Health. 2019;19(1): 1293.Figures
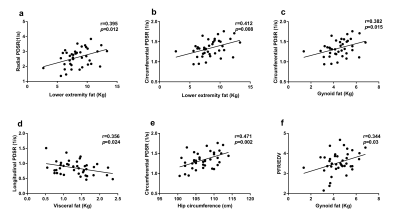
Figure 1. Association among regional fat distributions and LV diastolic parameters in patients with obesity. (a) and (b) lower extremity fat vs. radial PDSR and circumferential PDSR, respectively, (c) gynoid fat vs. circumferential PDSR, (d) visceral fat vs. longitudinal PDSR, (e) hip circumference vs. circumferential PDSR, and (f) gynoid fat vs. PFR/EDV. PDSR= peak diastolic strain rate
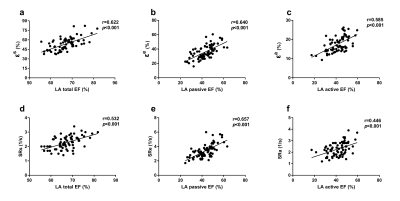
Figure 2. Bivariate correlations of left atrial function derived from the volumetric analysis and corresponding longitudinal strain parameters of CMR-tissue tracking. (a) LA total EF vs. εs, (b) LA passive EF vs. εe, (c) LA active EF vs. εa, (d) LA total EF vs. SRs, (e) LA passive EF vs. SRe, (f) LA active EF vs. SRa. EF=emptying fraction, εs=total strain, εe=passive strain, εa=active strain, SRs=peak positive strain rate, SRe=peak early negative strain rate, SRa=peak late negative strain rate
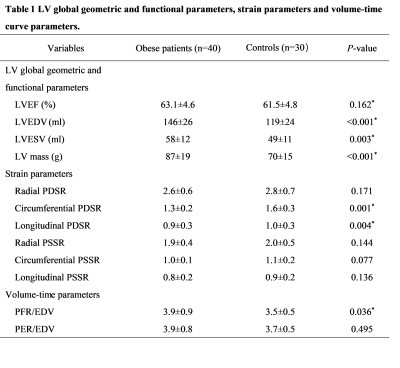
Table 1 LV global geometric and functional parameters, strain parameters and volume‑time curve parameters. LV = left ventricular; EF = ejection fraction; EDV = end diastolic volume; ESV = end systolic volume; PDSR= peak diastolic strain rate; PSSR = peak systolic strain rate; PFR = peak filling rate; PER = peak ejection rate. * p < 0.05
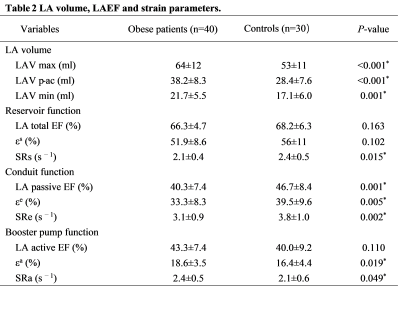
Table 2 LA volume, LAEF and strain parameters. LA = left atrium; EF = emptying fraction, Vmax = maximum volume, Vpre-a = pre-atrial contraction volume, Vmin = minimum volume, εs = total strain, εe = passive strain, εa = active strain, SRs = peak positive strain rate, SRe = peak early negative strain rate, SRa = peak late negative strain rate. * p < 0.05
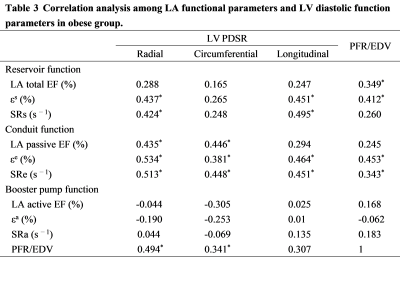
Table 3 Correlation analysis among LA functional parameters and LV diastolic function parameters in obese group. LA = left atrium; EF = emptying fraction, εs = total strain, εe = passive strain, εa = active strain, SRs = peak positive strain rate, SRe = peak early negative strain rate, SRa = peak late negative strain rate; PDSR= peak diastolic strain rate; PFR = peak filling rate; EDV = end diastolic volume. * p < 0.05