4163
Regional fat distributions are associated with subclinical right ventricular dysfunction in adults with uncomplicated obesity1Radiology, West China Hospital, Sichuan University, Chengdu, China, 2Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, China, 3MR Collaboration, Siemens Healthineers Ltd., Shanghai, China
Synopsis
This study evaluated right ventricular (RV) functional changes using cardiac magnetic resonance (CMR) tissue tracking and the association of these changes with fat distributions in obese adults with no clinical signs or comorbidities. The results showed that CMR tissue tracking can detect subclinical RV dysfunction with preserved RV ejection fraction in obese adults. Central obesity, represented by android fat, trunk fat, and the android/gynoid fat mass ratio, had a deleterious effect on RV subclinical dysfunction, whereas peripheral obesity (gynoid fat) might have had a protective effect. These findings could contribute to more precise obesity management in clinical practice.
Introduction
The number of overweight and obese people has increased rapidly over the last decades which has caused an increase in the global disease burden. To date, no country has successfully reversed this obesity epidemic1, 2. Previous studies examining cardiac function and the cardiovascular system have mainly focused on obese patients with comorbidities, such as diabetes, hypertension, and coronary heart disease, while little research has focused on obese subjects with no clinical signs or comorbidities. Specific right ventricular (RV) functional changes on cardiac magnetic resonance (CMR) have not been studied in this subset of obese patients.Echocardiography is widely used to assess ventricular function. In subjects with obesity, signal interference due to excessive adiposity makes echocardiography challenging. The advantages of CMR include access to larger fields of view, higher signal-to-noise ratios, and 3-dimensional imaging of the heart, allowing for ventricular geometry and functional assessments with high accuracy and reproducibility3. Currently, the CMR tissue tracking technique has been applied as a subclinical myocardial dysfunction indicator because of its high sensitivity when measuring global and regional cardiac mechanics through tracking myocardial motion4. Dual X-ray absorptiometry (DXA) has also been extensively applied as it allows the accurate assessment of regional fat distributions, such as fat of the android, gynoid, trunk, upper and lower extremities, and visceral regions. We aimed to evaluate RV functional changes seen on CMR tissue tracking and determine the association of these changes with fat distributions in adults with uncomplicated obesity.
Methods
This study prospectively recruited 49 obese participants (BMI≥ 27.5 kg/m2) and 30 healthy controls (18.5 ≤ BMI ≤ 23.5 kg/m2) between 18 and 60 years old, who underwent CMR on a 3T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). Subjects were excluded if they had any of the following conditions: hypertension or diabetes measured by oral glucose tolerance; history of cardiovascular diseases or history of any cardiovascular procedures; major systemic diseases that could affect the myocardium, such as connective tissue diseases and sarcoidosis; endocrine disease, such as hyperthyroidism and hypothyroidism; metabolic diseases, such as a history of alcohol abuse or amyloidosis; obstructive sleep apnea; and any contraindication to CMR imaging. A segmented breath-hold balanced steady-state free precession (bSSFP) sequence was used to obtain 8–14 contiguous cine images from the base to the apex in the short-axis view and two- and four-chamber cine images in the long-axis view. The bSSFP parameters were as follows TR/TE=3.3/1.22 ms, flip angle=41°, slice thickness=8 mm, field of view=360 × 320 mm2, matrix size=208 × 166, and a temporal resolution=39.34 ms. Body fat distributions were measured with dual X-ray absorptiometry. RV functional indices of participants with obesity were compared with those of controls. Correlations among related body fat distributions and RV function indices were conducted with multivariable linear regression.Results
Compared with controls, obese participants had impaired RV strain parameters with lower global longitudinal peak strain (PS), circumferential and longitudinal peak systolic strain rates (PSSR), and peak diastolic strain rates (PDSR) (all p <0.05), while LV and RV ejection fractions(EFS)were not significantly different between the two groups (p >0.05). The obese subjects had cardiac remodeling with greater RV size, LV myocardial mass, and LV wall thickness compared with the controls. Multivariable linear regression controlling for sex, age, height, and systolic blood pressure showed that android and trunk fat were inversely correlated with circumferential PS and circumferential strain rates (PSSR and PDSR) (Android fat-circumferential PS, PSSR and PSDR: β = -1.513, β = -0.081, and β = -0.131, respectively; trunk fat-circumferential PS, PSSR and PSDR: β = -0.344, β = -0.021, and β = -0.028, respectively; all p <0.05). The android/gynoid fat mass ratio (A/G fat ratio) was negatively associated with circumferential PS (β = -7.308, p= 0.006). In contrast, gynoid fat was positively associated with longitudinal PDSR (β = 0.068, p = 0.044). Upper and lower extremities fat were not significantly associated with RV function (p >0.05). Central fat deposits, represented by android fat, the A/G fat ratio, and visceral fat, were positively correlated with triglycerides (r = 0.3 to 0.6), while the A/G fat ratio and visceral fat were negatively correlated with HDL (r = -0.470 and r = -0.429). In contrast, peripheral fat deposits, represented by gynoid fat and lower extremity fat, were positively associated with HDL (r = 0.303 and r = 0.343).Discussion and Conclusions
This study compared RV functional parameters in obese adults with those in normal controls and revealed an association of these changes with fat distributions in obese adults with no clinical signs or comorbidities. CMR tissue tracking could detect subclinical RV dysfunction with preserved RVEFs in uncomplicated obese adults. Central obesity (android fat, trunk fat, and A/G fat ratio) has a deleterious effect on RV subclinical dysfunction, while peripheral obesity (gynoid fat) might have had a protective effect. A partial explanation for this result was that regional fat distributions can affect dyslipidemia differently. These findings could help with obesity management in clinical practice.Acknowledgements
This work was supported by the National Natural Science Foundation of China [Grant number. 81601462], the Key Research & Development Project of Science and Technology of Sichuan Province (Grant number. 21ZDYF1602), 1.3.5. project for disciplines of excellence, West China Hospital, Sichuan University (Grant number. ZYGD18017).
References
1. Collaborators GBDO, Afshin A, Forouzanfar MH, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13-27.
2. Swinburn BA, Kraak VI, Allender S, et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet. 2019;393(10173):791-846.
3. Grothues F, Smith GC, Moon JC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90(1):29-34.
4. Claus P, Omar AMS, Pedrizzetti G, Sengupta PP, Nagel E. Tissue Tracking Technology for Assessing Cardiac Mechanics: Principles, Normal Values, and Clinical Applications. JACC Cardiovasc Imaging. 2015;8(12):1444-1460.Figures
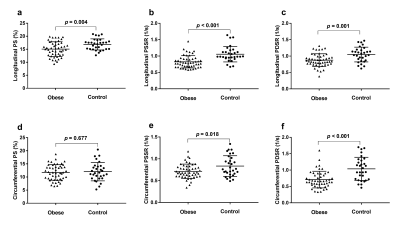
Figure 1: Dot plots comparing right ventricular strain parameters of obese patients and normal controls. (a), (b), and (c) longitudinal PS, PSSR, and PDSR; (d), (e) and (f) circumferential PS, PSSR, and PDSR. PS: peak strain; PSSR: peak systolic strain rate; PDSR: peak diastolic strain rate.
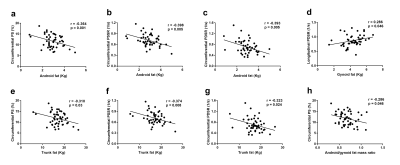
Figure 2: Correlations between regional fat distributions and right ventricular strain parameters in patients with obesity. (a), (b), and (c) android fat and circumferential PS, PSSR, and PDSR; (d) gynoid fat and longitudinal PDSR; (e), (f), and (g) trunk fat circumferential PS, PSSR, and PDSR; (h) android/gynoid fat mass ratio and circumferential PS. PS: peak strain; PSSR: peak systolic strain rate; PDSR: peak diastolic strain rate.
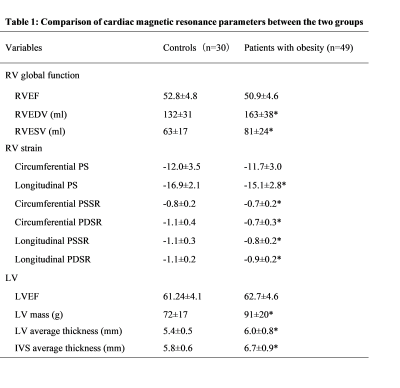
Table 1: Comparison of cardiac magnetic resonance parameters between two groups. RV = right ventricular; EF = ejection fraction; EDV = end diastolic volume; ESV = end systolic volume; PS = peak strain; PSSR = peak systolic strain rate; PDSR = peak diastolic strain rate; LV = left ventricular; IVS = interventricular septum. * p < 0.05
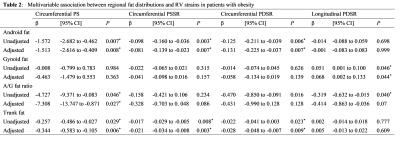
| Table 2: Multivariable association between regional fat distribution and RV strains in obese patients. PS = peak strain; PSSR = peak systolic strain rate; PDSR = peak diastolic strain rate; BMI = body mass index; A/G ratio = Android-to- gynoid ratio; CI = confidence interval Adjustment: age, sex, height, and systolic blood pressure for android fat, gynoid fat, A/G ratio and trunk fat. * p < 0.05 |
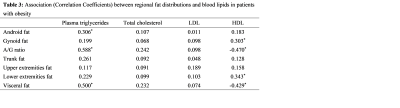
Table 3: Association (Correlation Coefficients) between regional fat distribution and blood lipids in patients with obesity. A/G fat ratio = Android-to- gynoid ratio; LDL = low-density lipoprotein; HDL = high-density lipoprotein. * p < 0.05