4161
Characteristics of left atrial strain in hypertrophic cardiomyopathy comorbid HF with preserved EF: evaluation by CMR-feature tracking1West China hospital of Sichuan University, Chengdu, China
Synopsis
The majority of heart failure (HF) in hypertrophic cardiomyopathy (HCM) manifests as a phenotype with preserved left ventricular (LV) ejection fraction, however, the exact contribution of left atrial (LA) phasic function to HF with preserved ejection fraction (HFpEF) in HCM remains unresolved. We designed the study to define the association between LA function and HFpEF in HCM patients using cardiac MRI feature tracking. The result revealed that LA phasic function was severely impaired in HCM patients with HFpEF, whereas LV function was not further impaired compared with non-HF patients.
Background
The majority of heart failure (HF) in hypertrophic cardiomyopathy (HCM) manifests as a phenotype with preserved left ventricular (LV) ejection fraction, however, the exact contribution of left atrial (LA) phasic function to HF with preserved ejection fraction (HFpEF) in HCM remains unresolved.Purpose
To define the association between LA function and HFpEF in HCM patients using cardiac MRI feature tracking.Method
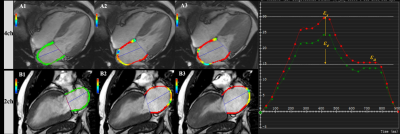
Population: 154 HCM patients (HFpEF vs. non-HF: 55(34 females) vs. 99(43 females)).Field strength/sequence: 3.0T/balanced steady-state free precession
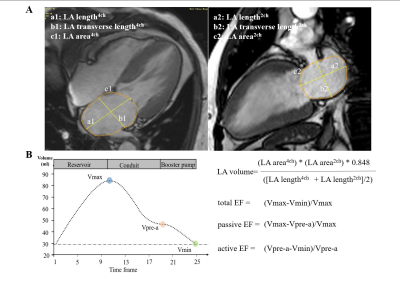
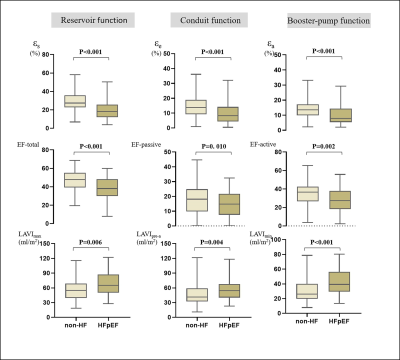
Assessment: LA reservoir function (reservoir strain (εs), total ejection fraction (EF)), conduit function (conduit strain (εe), passive EF), booster-pump function (booster strain (εa) and active EF), LA volume index, and LV global longitudinal strain (LV GLS) were evaluated in HCM patients.
Statistical Tests: Chi-square test, student’s t-test, Mann-Whitney U test, multivariate linear regression, logistic regression, and Net reclassification analysis were used, two-sided p<0.05 was considered statistically significant.
Results
No significant difference was found in LV GLS between the non-HF and HFpEF group (-10.67±3.14% vs. -10.14±4.01%, p=0.397), whereas the HFpEF group had more severely impaired LA phasic strain (εs:27.40[22.60,35.80] vs. 18.15[11.98,25.90]; εe:13.80[9.20,18.90] vs. 7.95[4.30,14.35]; εa: 13.50[9.90,17.10] vs. 7.90[5.40, 14.15]). LA total EF (37.91[29.54,47.94] vs. 47.49[39.18,55.01]), passive EF (14.70[7.41,21.49] vs. 18.07[9.32,24.78]), and active EF (27.19[17.79,36.60] vs. 36.64[26.63,42.71]) were all significantly decreased in HFpEF patients compared with non-HF patients. LA reservoir (β=0.90[0.85,0.96]), conduit (β=0.93[0.87,0.99]), and booster (β=0.86[0.78,0.95]) strain were independently associated with HFpEF in HCM patients. The model including reservoir strain (Net Reclassification Index (NRI): 0.260) or booster strain (NRI: 0.325) improved the reclassification of HFpEF based on LV GLS and minimum left atrial volume index (LVAImin).Discussion
This study focused on the association between HFpEF and LA phasic function in HCM. The main findings were: 1) HCM patients with HFpEF had severely impaired LA function and relatively preserved LV GLS compared with non-HF patients; 2) LAVImax was associated with LA reservoir, conduit, and booster strain in HCM patients independent of HF status; and 3) LA reservoir, conduit, and booster strain are independently associated with HFpEF in HCM patients. Compared with the conventional model, which only included LV GLS and LAVImin, LA reservoir and booster strain improve the reclassification ability of HFpEF in HCM patients.It should be noted that HCM-related HF contrasts sharply with conventional HFpEF 1. They are very different and heterogeneous conditions with different clinical presentations and pathophysiology. Myocardial fibrosis causes LA wall stiffness and results in decreased LA compliance in HCM patients has been confirmed 2,3. In our patients, left atrium function worsened as the HF symptoms developed; However, further left ventricular function impairment was not observed. It is reasonable to presume that LA dysfunction plays an essential role in developing HF symptoms in patients with HCM.
The predictive value of LAVImin in HF was verified in a recent study4. Our study showed that neither LAVImax nor LV GLS was associated with HFpEF in HCM patients. These findings are inconsistent with previous research. The most likely explanation is the different study populations in our study compared with previous research, which focused on other diseases that may result in myocardial injuries, such as hypertension and diabetes, rather than primary cardiomyopathy 5,6. We found that all LA phasic strains were independently associated with HFpEF, and only reservoir and booster strain improved reclassification ability based on LV GLS and LAVImin. A prior large cohort study pointed out the potential usefulness and clinical relevance of adding LA reservoir strain to LA volume in the detection of HFpEF 7. Our study adds to this body of evidence and further extends to HCM patients. Based on our findings, LA booster-pump strain decreased early and played an essential role in differentiating HFpEF from non-HF entities in HCM, which may be attributable to LA myocardial involvement accelerating the LA dysfunction.
Conclusions
LA phasic function was severely impaired in HCM patients with HFpEF, whereas LV function was not further impaired compared with non-HF patients.Acknowledgements
NAReferences
1. Maron BJ, Rowin EJ, Udelson JE, Maron MS. Clinical Spectrum and Management of Heart Failure in Hypertrophic Cardiomyopathy. JACC Heart failure 2018;6(5):353-363.
2. Sivalokanathan S, Zghaib T, Greenland GV, et al. Hypertrophic Cardiomyopathy Patients With Paroxysmal Atrial Fibrillation Have a High Burden of Left Atrial Fibrosis by Cardiac Magnetic Resonance Imaging. JACC Clinical electrophysiology 2019;5(3):364-375.
3. Pontecorboli G, Figueras IVRM, Carlosena A, et al. Use of delayed-enhancement magnetic resonance imaging for fibrosis detection in the atria: a review. Europace 2017;19(2):180-189.
4. Hinojar R, Zamorano JL, Fernández-Méndez M, et al. Prognostic value of left atrial function by cardiovascular magnetic resonance feature tracking in hypertrophic cardiomyopathy. Int J Cardiovasc Imaging 2019;35(6):1055-1065.
5. Kosmala W, Rojek A, Przewlocka-Kosmala M, Mysiak A, Karolko B, Marwick TH. Contributions of Nondiastolic Factors to Exercise Intolerance in Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol 2016;67(6):659-670.
6. Huang W, Chai SC, Lee SGS, MacDonald MR, Leong KTG. Prognostic Factors After Index Hospitalization for Heart Failure With Preserved Ejection Fraction. Am J Cardiol 2017;119(12):2017-2020.
7. Morris DA, Belyavskiy E, Aravind-Kumar R, et al. Potential Usefulness and Clinical Relevance of Adding Left Atrial Strain to Left Atrial Volume Index in the Detection of Left Ventricular Diastolic Dysfunction. JACC Cardiovasc Imaging 2018;11(10):1405-1415.
Figures