4147
The impact factors of the Quality of non-contrast agent Coronary angiography at 3.0T Magnetic Resonance
Junjing He1, Xiuzheng Yue2, Gang Zhang1, Wei Xing1, Tingting Li1, Yufu Hu1, and Yuhan Wang1
1Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 2Philips Healthcare, Beijing, China
1Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 2Philips Healthcare, Beijing, China
Synopsis
This study explores impact factors of the quality of 3.0T non-contrast agent magnetic resonance coronary angiography (MRCA), and uses an objective standard for assessing the image quality. A retrospective review was conducted on 72 patients who successfully completed 3.0T MRCA, and the correlation between their image quality and their clinical data, scan sequence, parameter settings, imaging technology and other factors were analyzed.The study found that BMI and respiratory motion were the key factors that affect the quality of non- contrast agent coronary MRA on 3.0T MRI. The mDixon-TFE imaging method can be used for MRCA as a routine scanning sequence.
Introduction
In the past ten years, magnetic resonance coronary angiography (MRCA) imaging has developed rapidly. It is now being gradually promoted from scientific research to clinical use. The advantages of CMRA are no ionizing radiation, non-contrast agent injection and better tissue contrast for angiography. Compared with other anatomical parts, the coronary artery lumen is small, and its spatial anatomical structure is complex[1].MRCA has unique value in the diagnosis of coronary artery disease, and its clinical needs are gradually increasing. However, the current technology lacks objective standards for assessing the image quality and impact factors. In addition, this study also found that the patients’ own physiological and pathological factors, scan sequence, parameter settings, and imaging technology will also affect the quality of coronary imaging. And the purpose of this study is to analyze the factors that may affect the quality of MRCA imaging promoting the application of MRCA in clinical practice.Methods
A total of 72 patients (32 women; average age ± standard deviation: 56 ± 14 years) who successfully underwent whole-heart MRCA examination data were included in this study. All patients had three visible MRCA images and could be used for clinical diagnosis.All patients were scanned using a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands) with a 32-channel dS Anterior coil is used for the coil.In this study, two imaging methods of mDixon and BTFE were used for whole-heart scanning. The scanning parameters of mDixon were: TR: shortest, TE first: shortest, acquisition matrix, 176×201; voxel size, 1.5×1.5mm; slice thickness, 1.5 mm; 140 axial slices; flip angle=10°.BTFE scanning parameters are: scanning parameters: TR: shortest, TE first: shortest, acquisition matrix, 280×259; voxel size, 1.25×1.35mm; slice thickness, 1.5 mm; 140 axial slices; flip angle=17°All participants’ coronary images will be subjectively and objectively scored. Two experienced and senior physicians rated their images as excellent based on factors such as the visual perception of the coronary artery, the sharpness of the lumen and the severity of artifacts. The data are rated for four grades. Objectively scoring: Obtaining six regions of interest (ROI) of equal area in the mid-segment of the coronary artery in mDIXON sequence and measuring the signal intensity and background noise standard deviation of the coronary artery and aorta in the region of interest. The calculation method [3] is: CRtissue1/tissue2=|μtissue1-μtissue2|/√σtissue12+σtissue22.Convert the measured value into a signal intensity standardized contrast ratio (contrast raito, CR) [2],is the coronary signal intensity,is the aortic signal intensity of the same layer,is the standard deviation of the coronary signal,is the standard deviation of the aortic signal of the same layer.One-way analysis of variance was used to determine the difference in CR values between the subjective scores. The impact factors of image quality were analyzed by ordered logistic regression, and P<0.05 indicated that the difference was statistically significant.Results
The CR value of the excellent group image is 2.62±1.69, the CR value of the good group image is 2.97±2.18, the CR value level of the middle group image is 3.63±2.83, and the CR value of the poor group image is 4.06± 2.82, the difference in CR values between the good and the poor groups was statistically significant (P<0.001); there was no correlation between gender composition, age difference, blood pressure, heart rate, ejection fraction, stroke volume, and image quality ( P>0.05), while BMI and collection efficiency (group 2=40-60%) are related to the image quality (P<0.05), and there is a negative correlation between BMI and image quality. There is a positive correlation between acquisition efficiency and image quality; the patient’s own physiological and pathological factors, scanning sequence, parameter settings and different imaging technologies will also affect the quality of coronary imaging.Discussion
CR value can reflect the difference between the pros and cons of images and has good consistency with the subjective score, which can be used as an objective index to evaluate the image quality. There is a clear correlation between BMI and image quality [3]. With the increase of BMI, the unfavorable factors for MRCA imaging also increase correspondingly. Although there is an obvious correlation between the acquisition efficiency of 40%-60% and the image quality [4], we believe that the acquisition efficiency reflects the external performance of the patient’s breathing movement that affects the image acquisition, which can be used as an important technical adjustment in the scanning process. The patient's physio pathological factors, scan sequence, parameter settings and different imaging techniques will also affect the quality of MRCA images. However, there are relatively few reports in domestic and foreign literature on this aspect, and further research and improvement are needed. In the future, the sampling points of diaphragm movement can be optimized [5] and the algorithm of compressed SENSE technology [6] to shorten the acquisition time and improve Image quality [7].Conclusion
At this stage, MRCA imaging technology is relatively complicated. The complexity is not the scanning positioning, but the individual's plan. During the scanning process, the corresponding plan and parameters must be formulated according to the characteristics of the patient, and finally high-quality images can be obtained. BMI and respiratory methods are the key factors that affect MRCA images. mDixon imaging method can be used as a routine scanning sequence [8].Acknowledgements
No acknowledgement found.References
[1] Ishida M, Sakuma H. Coronary MR angiography revealed: how to optimize image quality. Magn Reson Imaging Clin N Am. 2015;23(1):117-125. doi:10.1016/j.mric.2014.09.008.[2] Ding J, Duan Y, Zhuo Z, et al. Acceleration of Brain TOF-MRA with Compressed Sensitivity Encoding: A Multicenter Clinical Study. AJNR Am J Neuroradiol. 2021;42(7):1208-1215. doi:10.3174/ajnr.A7091.[3] Dai Jingwen. The diagnostic value of 3.0T magnetic resonance coronary angiography for coronary heart disease[D]. Peking Union Medical College, 2019.[4] He Y, Pang J, Dai Q, Fan Z, An J, Li D. Diagnostic Performance of Self-navigated Whole-Heart Contrast-enhanced Coronary 3-T MR Angiography [published correction appears in Radiology. 2017 Jun;283(3):923]. Radiology. 2016;281(2):401-408. doi:10.1148/radiol.2016152514[5] Addy NO, Ingle RR, Luo J, et al. 3D image-based navigators for coronary MR angiography. Magn Reson Med. 2017;77(5):1874-1883. doi:10.1002/mrm.26269[6] Wech T, Lemke A, Medway D, et al. Accelerating cine-MR imaging in mouse hearts using compressed sensing. J Magn Reson Imaging. 2011;34(5):1072-1079. doi:10.1002/jmri.22718[7] Hajhosseiny R, Bustin A, Munoz C, et al. Coronary Magnetic Resonance Angiography: Technical Innovations Leading Us to the Promised Land?. JACC Cardiovasc Imaging. 2020;13(12):2653-2672. doi:10.1016/j.jcmg.2020.01.006[8] Lu H, Guo J, Zhao S, et al. Assessment of Non-contrast-enhanced Dixon Water-fat Separation Compressed Sensing Whole-heart Coronary MR Angiography at 3.0 T: A Single-center Experience [published online ahead of print, 2021 Jun 11]. Acad Radiol. 2021;S1076-6332(21)00224-5. doi:10.1016/j.acra.2021.05.009Figures
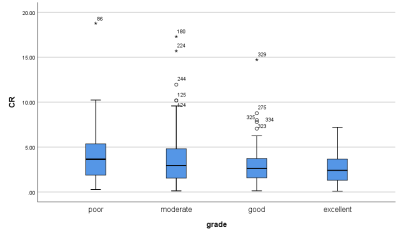
Figure 1. Consistency analysis of subjective and objective ratings and image quality.The grade represents the subjective score, which is divided into four groups: excellent, moderate and poor.
Table 1. Correlation analysis of patients' general clinical data and image quality
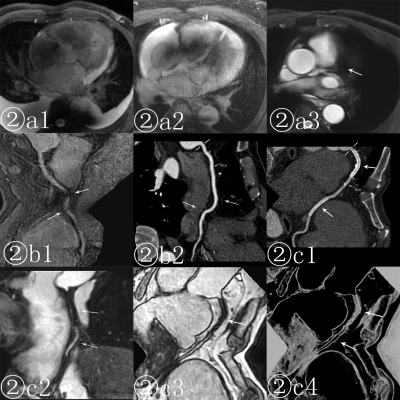
Figure ②a shows the effect of thoracic and lung diseases on coronary MRCA imaging; Figure ②b represents the influence of heart rate and hemodynamics on image quality; Figure ②c shows that MRCA has the possibility of evaluating patients after stenting.
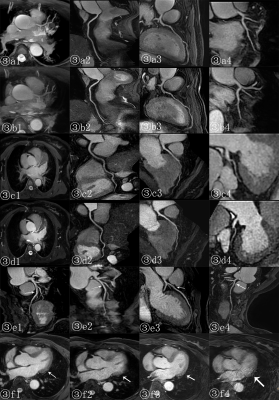
③a③b reflects the visual difference caused by the application of different imaging methods; ③c③d reflects the image difference caused by different T2-prep pulse settings; ③e reflects the differences in the image performance of different imaging methods at the vascular bifurcation; ③f reflects the difference It is the image difference under different acceleration factors and the artifacts that may be associated with this technology.
DOI: https://doi.org/10.58530/2022/4147