4116
Diagnostic value of NCE-CMRA in detection of inflammatory factors related coronary artery damage in Kawasaki disease1Department of Magnetic Resonance, Lanzhou University Second Hospital, Lanzhou, China, 2Philips Healthcare, Xi'an, China
Synopsis
This study mainly uses the non-contrast whole-heart magnetic resonance coronary angiography (NCE-CMRA) to evaluate coronary artery lesion (CAL) in children with Kawasaki disease (KD), and analyze the mechanism of inflammatory factors in the occurrence and development of coronary artery lesions in KD. Multiple linear regression was used to analyze the correlation between inflammatory factors and the severity of CAL. Platelet, PCT, ESR, CRP, D-dimer, albumin, and leukocyte have certain diagnostic value for KD, among which ESR is the most sensitive. Therefore, NCE-CMRA combined with inflammatory indicators is helpful for early diagnosis and prognostic evaluation of CAL in children with KD.
Introduction
Kawasaki disease (KD) is an acute non-specific arterial vasculitis and has become the main cause of acquired heart disease in children. The long-term prognosis of KD mainly depends on the involvement of the coronary artery. Non-contrast whole-heart magnetic resonance coronary angiography (NCE-CMRA) can effectively evaluate coronary artery involvement. Besides, another important method to evaluate coronary artery lesion (CAL) is to observe the changes of KD-related inflammatory factors. Early detection of the changes of inflammatory factors is helpful to predict the damage of coronary artery as soon as possible1. This study evaluates the diagnostic value of NCE-CMRA in KD with CAL, and explore the correlation between KD related inflammatory factors and the occurrence and development of CAL.Materials and Methods
Fifty-two children who were clinically diagnosed with KD in Lanzhou University Second hospital from June 2017 to June 2020 were analyzed retrospectively. There were 32 males and 20 females, aged from 9 months to 11 years, with an average of 5.9 ± 0.3 years old. All cases met the 2017 KD diagnostic criteria of the American Heart Association2. The images of all children were collected using Philips Ingenia 3.0T MR scanner with 16-channel body phased array coil. The scan sequence was 3D-TFE-NAV combined with ECG gating technology triggered by R-wave and diaphragm navigation. The FOV was 300x250 mm2, the number of slices was 100-120, the acquisition voxel was 1.25x1.25x1.6 mm3, and the reconstruction voxel was 0.62x0.62x0.8 mm3. Meanwhile, the frequency selection method was used to suppress the fat signal to enhance the contrast of the coronary artery signal. Then the subjects were divided into the normal coronary artery (NCAL) group (16 cases, F/M: 4/12) and the coronary artery lesion (CAL) group (36 cases, F/M: 16/20). The differences of inflammatory indices between the two groups were compared, and the sensitivity of inflammatory indices was analyzed by ROC curve. Multiple linear regression was used to analyze the correlation between each inflammatory factor and the severity of CAL. All statistical analysis is realized by SPSS software.Results
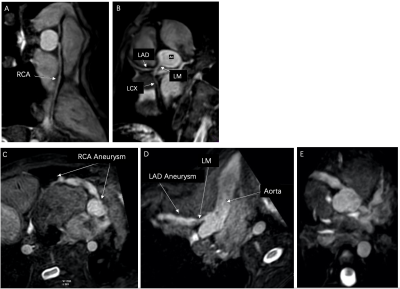
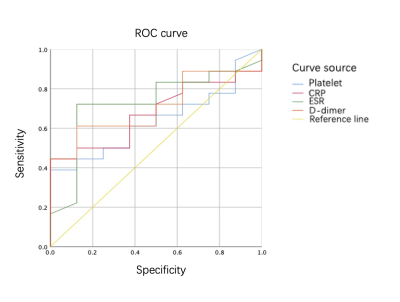
As can be seen in figure 1, the coronary arteries in the NCAL group were normal, and all branches were not involved (A, B). On the contrary, the coronary arteries in the CAL group were widened, multiple aneurysms were found (C, D, E). Among the inflammatory indices of 52 children, the positive rates of platelet, PCT, ESR, CRP, D-dimer, albumin and leukocyte were 76.9%, 69.2%, 69.2%, 50%, 50%, 46.1% and 34.6% respectively. Statistical analysis showed that the levels of PLT, CRP, ESR, and D-dimer in the CAL group were significantly higher than those in the NCAL group (P <0.05). The sensitivities of ESR, D-dimer, CRP and PLT were 72%, 61%, 44%, and 39% respectively (table1, figure 2). In the CAL group, PLT, CRP, D-dimer were positively correlated with the ratio of the affected vessel diameter, among which CRP was significantly correlated; ESR had a certain correlation with the length of involved and the number of involved vessels, as shown in table 2.Discussion
NCE-CMRA is a reliable technology in displaying coronary artery lesions and distal branches. It can accurately describe the degree of coronary artery disease, which is convenient for CAL risk rating3. Studies have shown that a variety of inflammatory factors are involved in the occurrence and development of KD and the evaluation of CAL caused by KD is related to the level of inflammatory factors4. The results of this study showed that PLT, PCT, ESR and IL-6 had the most diagnostic value in coronary artery injury in children with KD. The levels of PLT, CRP, ESR, and D-dimer in the CAL group were significantly higher than those in the NCAL group suggesting that the occurrence of CAL is related to the increase of inflammatory factors, among which ESR is the most sensitive one. PLT is one of the factors that mediate systemic inflammatory response, and it can release inflammatory mediators such as chemokines and cytokines which results the intensification of inflammatory response5. D-dimer is one of the molecular markers of thrombosis and fibrinolysis activation, and it is the most commonly used indicator of activation of the coagulation system6. A number of studies have shown that D-dimer gradually increases after the onset of KD in children, so changes in the level of D-dimer are of great value for the diagnosis of CAL in KD. When KD develops to the advanced stage, the coronary arteries are exposed to high inflammation environment for a longer time, the range of coronary artery lesions and the number of vessels involved in the lesions will increases, and the sedimentation rate of red blood cells will be significantly accelerated, which in turn affects ESR7. Therefore, ESR can reflect the overall damage of coronary artery to a certain extent.Conclusion
NCE-CMRA can objectively and accurately show the imaging characteristics and severity of coronary artery lesions in children with KD. The PLT, CRP, ESR, and D-dimer are the high-risk factors for KD with CAL, among which ESR is the most sensitive one. Therefore, the combination of NCE-CMRA and inflammatory indicators is helpful for the early diagnosis and prognostic evaluation of coronary artery disease in children with KD.Acknowledgements
No acknowledgement found.References
1. Pavd A, Mjb A, Rsd A, et al. Prognostic Value of RCA Pericoronary Adipose Tissue CT-Attenuation Beyond High-Risk Plaques, Plaque Volume, and Ischemia[J]. JACC: Cardiovascular Imaging, 2021.
2. Mccrindle B W, Rowley A H, Newburger J W, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association[J]. Circulation, 2017, 135(17):e927.
3. Kim J W, Goo H W. Coronary artery abnormalities in Kawasaki disease: comparison between CT and MR coronary angiography[J]. Acta Radiologica, 2013, 54(2):156-63.
4. Jin J, Wang J, Lu Y, et al. Platelet-Derived Microparticles: A New Index of Monitoring Platelet Activation and Inflammation in Kawasaki Disease[J]. Indian Journal of Pediatrics, 2019.
5. Balta S, Demrkol S, Kucuk U. The platelet lymphocyte ratio may be useful inflammatory indicator in clinical practice[J]. Hemodialysis International, 2013, 17(4):668-669.
6. Masuzawa Y, Mori M, Hara T, et al. Elevated D-dimer level is a risk factor for coronary artery lesions accompanying intravenous immunoglobulin-unresponsive Kawasaki disease[J]. Therapeutic apheresis and dialysis: official peer-reviewed journal of the International Society for Apheresis, the Japanese Society for Apheresis, the Japanese Society for Dialysis Therapy, 2015, 19(2).
7. Song X Y, Huang J Y, Hong Q, et al. Platelet count and erythrocyte sedimentation rate are good predictors of Kawasaki disease: ROC analysis[J]. Journal of Clinical Laboratory Analysis, 2010, 24(6):385-388.
Figures