4019
An Interactive App with Multi-parametric MRI - Whole Mount Histology Correlation for Enhanced Prostate MRI Training of Radiologists1Department of Radiology, University of Chicago, Chicago, IL, United States, 2Sanford J. Grossman Center of Excellence in Prostate Imaging and Image Guided Therapy, Chicago, IL, United States, 3Research Computing Center, University of Chicago, Chicago, IL, United States, 4C. Wheeler Studios, Chicago, IL, United States
Synopsis
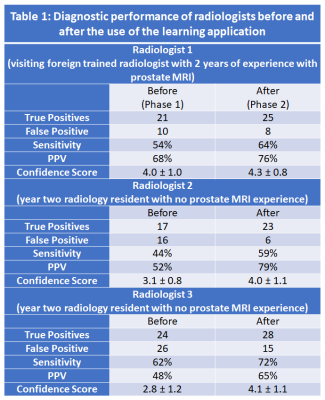
We created an interactive application Learn Radiology with multi-parametric MRI - whole mount histology correlation for enhanced prostate MRI training of radiologists and validated whether the use of a newly created learning application can enhance prostate MRI training of radiologists using an observer study. Sensitivity (R1: 54%→64%, R2: 44%→59%, R3: 62%→72%), PPV (R1: 68%→76%, R2: 52%→79%, R3: 48%→65%) and confidence score (R1: 4.0±1.0→4.3±0.8, R2: 3.1±0.8→4.0±1.1, R3: 2.8±1.2→4.1±1.1, p<0.05) for prostate cancer diagnosis using mpMRI improved for all three radiologists along with inter-observer agreement (α 0.78→0.85) after being exposed to our developed teaching app.
Introduction
Diagnosing prostate cancer remains challenging for radiologists due to the complex multi-parametric (mpMRI) approach where radiologists are expected to compare multiple complex two-dimensional modalities with one another and then translate the found pathology back into the patient’s prostate in three dimensions. This can be challenging, especially if one’s spatial ability is limited. Saha et al (1), found that less than 35% of year one radiology residents showed any confidence in image diagnosis. Web-based, 3D models and interactive e-learning resources can support higher education and have begun playing a pivotal role in the evolution of medical education and the way residents prepare for rotations and examinations (2-4). The current modules that teach about MRI use patient cases, but still lack the application to real-world, clinical settings that include the mpMRI approach and the content necessary to improve the user’s visual memory and spatial ability for PCa diagnosis. Therefore, in this study we aimed to create an interactive application with multi-parametric MRI - whole mount histology correlation for enhanced prostate MRI training of radiologists and validated whether the use of a newly created learning application can enhance prostate MRI training of radiologists using an observer study.Materials and Methods
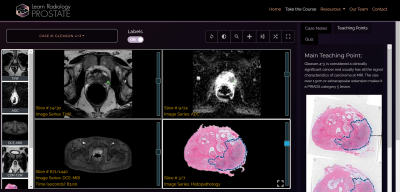
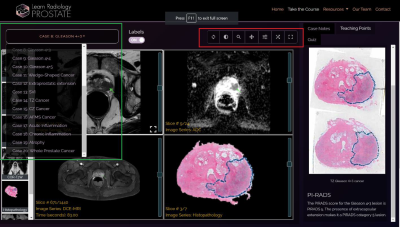
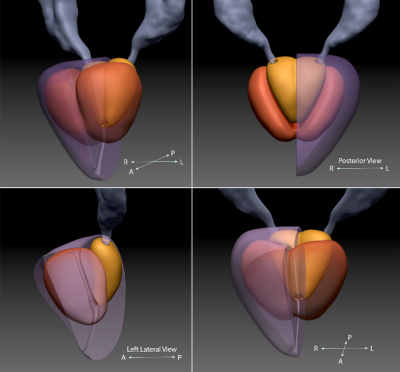
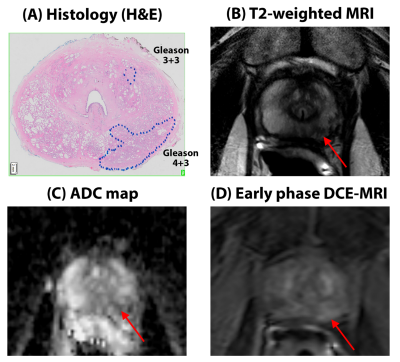
In this prospective study, an interactive learning application- LearnRadiology was developed using a web-based framework to display multi-parametric prostate MRI images with correlated whole mount histology for 20 cases curated for unique pathology and teaching points as shown in Figures 1 and 2. The use of histology images along with whole set of MR images and 3D prostate outlines (Figure 3) are novel in radiology training. The curated cases include 20 unique pathology findings that radiologist will likely encounter in their career. These include normal prostate, cancers with different Gleason score (3+3, 3+4, 4+3, 4+4, 4+5), at different locations (anterior, transition, peripheral zones), seminal vesicle invasion, extra prostatic extension as well other benign features that mimic cancer (inflammation, BPH types, atrophy, etc.).20 new prostate MRI cases (mean age 58±7 years, PSA 7.9±5.5 ng/mL), different from the ones used in the web-app were uploaded on 3D-Slicer. Three radiologists (R1: visiting foreign trained radiologist with 2 years of experience with prostate MRI, R2 and R3: year two radiology residents with no prostate MRI experience) blinded to pathology results were asked to mark areas suspected of cancer and provide a confidence score (1-5, with 5 being high confidence level). Then after a minimum memory washout period of 1 month, the same radiologists used the learning app and then repeated the same observer study. The diagnostic performance for detecting cancers (sensitivity and positive predictive value) before and after accessing the learning app was measured by correlating MRI with whole mount pathology by an independent reviewer.
Phase 1: Review 20 cases (study cases) → 1 month break for memory washout → review the leaning web app – Learn Radiology (curated cases with unique pathology) → Phase 2: review the same 20 cases (study cases)
Results
The 20 subjects included in the observer study had 39 cancer lesions (13 Gleason 3+3, 17 Gleason 3+4, 7 Gleason 4+3 and 2 Gleason 4+5 lesions, meeting minimum size of 5mm × 5mm).The sensitivity (R1: 54%→64%, R2: 44%→59%, R3: 62%→72%) and PPV (R1: 68%→76%, R2: 52%→79%, R3: 48%→65%) for detecting all cancers improved for all three radiologists after being exposed to the teaching app. The confidence score for true positive cancer lesion also improved significantly (R1: 4.0±1.0→4.3±0.8, R2: 3.1±0.8→4.0±1.1, R3: 2.8±1.2→4.1±1.1, p<0.05). Detailed results can be found in Table 1 with representative example in Figure 4.
The inter-observer agreement (Cronbach’s alpha) was higher after the users used the learning app, with strong agreement between readers found after using the app (α = 0.85) compared to only moderate or acceptable agreement (α = 0.78) earlier.
Similar results were seen if only clinically significant cancer (≥ Gleason 3+4) were considered. The sensitivity (R1: 73%→77%, R2: 54%→69%, R3: 73%→84%) and confidence score (R1: 4.2±0.9→4.4±0.8, p<0.001, R2: 3.2±0.8→4.1±1.1, p<0.001, R3: 3.0±1.3 → 4.2±1.1, p<0.001) for all three radiologists improved after being exposed to the teaching app.
Discussion
Web-based and interactive learning resources can support higher education, with improved diagnostic performance for detecting prostate cancer shown by radiologists after using our developed LearnRadiology app. The use of histology images along with whole set of MR images and 3D prostate outlines are novel in radiology training. The use of the web app to improve diagnostic performance was validated in an observer study using a radiologist showing improved sensitivity, PPV and confidence score in diagnosing prostate cancer using mpMRI. These results are consistent with studies with dedicated learning course using conventional methods for both radiologists and urologists (5-7). Therefore, Learn Radiology being an interactive and self-directed learning tool is well suited for improving readers’ performance with interpreting prostate mpMRI. Future studies may consider using artificial intelligence to further augment radiology education by aiding in the learning process and for precision education in radiology (8).Conclusion
Web-based and interactive learning resources can support higher education, with improved diagnostic performance for detecting prostate cancer shown by radiologists after using our developed LearnRadiology app.Acknowledgements
This study is funded by Radiological Society of North America (RSNA) Education Scholar Grant (ESCH1805) - An Interactive App with Multi-parametric MRI - Whole Mount Histology Correlation for Enhanced Prostate MRI Training of Radiologists (PI- Chatterjee)References
1. Saha A, Roland RA, Hartman MS, Daffner RH. Radiology Medical Student Education. Academic Radiology. 20(3):284-9.
2. Bedi HS, Yucel EK. “I Just Bought My Residents iPads… Now What?” The Integration of Mobile Devices Into Radiology Resident Education. American Journal of Roentgenology. 2013; 201(4):704-9.
3. Berney S, Bétrancourt M, Molinari G, Hoyek N. How spatial abilities and dynamic visualizations interplay when learning functional anatomy with 3D anatomical models. Anatomical Sciences Education. 2015; 8(5):452-62.
4. Williamson KB, Gunderman RB, Cohen MD, Frank MS. Learning Theory in Radiology Education. Radiology. 2004; 233(1):15-8.
5. Akin O, Riedl CC, Ishill NM, Moskowitz CS, Zhang J, Hricak H. Interactive dedicated training curriculum improves accuracy in the interpretation of MR imaging of prostate cancer. European Radiology. 2010; 20(4):995-1002.
6. Kasivisvanathan V, Ambrosi A, Giganti F, et al. A Dedicated Prostate MRI Teaching Course Improves the Ability of the Urologist to Interpret Clinically Significant Prostate Cancer on Multiparametric MRI. European Urology. 2019; 75(1):203-4.
7. Rosenkrantz AB, Ayoola A, Hoffman D, et al. The Learning Curve in Prostate MRI Interpretation: Self-Directed Learning Versus Continual Reader Feedback. American Journal of Roentgenology. 2016; 208(3):W92-W100.
8. Duong MT, Rauschecker AM, Rudie JD, et al. Artificial intelligence for precision education in radiology. The British Journal of Radiology. 2019; 92(1103):20190389.
Figures