4017
Multi-Shot Diffusion-Weighted Imaging of the Breast in the Supine Position1Radiology, Stanford University, Stanford, CA, United States, 2General Electric Healthcare, Botson, MA, United States
Synopsis
Diffusion-Weighted Imaging (DWI) in the supine position may provide a non-invasive, comfortable, and efficient MRI for breast cancer screening. The strong performance of multi-shot DWI in prone breast MRI has been established. However, supine breast MRI has increased motion, specific B0-inhomogeneity, and cardiac artifacts, all of which may affect multi-shot DWI. This work investigates supine multi-shot DWI of the breast with a flexible array coil. High image quality is achieved and the effects of number of shots and respiratory-gating are delineated. B0-inhomogeneity and ADCs in the supine position are reported including the potential effect of cardiac artifact on ADC measurement.
Introduction
Contrast-Enhanced (CE) Breast MRI performed in the supine position could be advantageous for alignment of findings with interventional procedures during diagnosis and treatment (1, 2). Supine breast MRI could also be beneficial for screening due to an increase in patient comfort and ease of positioning. Multi-shot Diffusion-Weighted Imaging (DWI) provides high image quality in the prone position and DWI may allow breast MRI screening without a contrast injection (3-5). In combination, Supine DWI has the potential to provide a non-invasive, comfortable and efficient breast MRI screening exam. In this work we investigate the performance of multi-shot DWI of the breast in the supine position.Methods
Volunteers and ProtocolTen volunteers were recruited for the study and provided written informed consent. The protocol included four multi-shot, MUltiplexed Sensitivity Encoding (MUSE) DWI acquisitions: 2-shot and 4-shot each with free breathing (FB) and respiratory gating (RG) (6). GRE-IDEAL was acquired for B0 inhomogeneity measurement and FSE for distortion assessment (7). All exams were performed on a 3T Premier (GE Healthcare, Waukesha, WI) using 15-channels of a 30-channel flexible array AIR coil (GE Healthcare, Waukesha. WI). Sequence imaging parameters are reported in Table 1.
B0 Inhomogeneity
B0 inhomogeneity affects the degree of distortion in DWI and will vary based on patient positioning. B0 maps were reconstructed from GRE-IDEAL. The left and right breast were segmented and the B0 absolute offset and variation were measured.
Apparent Diffusion Coefficient
Apparent Diffusion Coefficient (ADC) was measured in fibroglandular tissue in two slices per case, one adjacent to the heart and a second superior to the heart. Mean and standard deviation of the ADC in each ROI was calculated. Effects of FB/RG, slice location, and number of shots were assessed by a mixed-effects regression model.
Observer Study
Three radiologists performed a blinded observer study to assess the performance of MUSE in the supine position. Features sharpness, aliasing, perceived SNR, and overall image quality were rated on a scale from one (poorest performance) to five (highest performance). Effects of feature, free-breathing versus respiratory-gating and number of shots were assessed by a mixed-effects logistic regression of dichotomized (4/5 vs 1/2/3) ratings. Agreement among observers’ ratings was assessed by Gwet’s AC (8). A distortion assessment was performed on the b = 0 s/mm2 images and in comparison to the aligned slice on the FSE T2-weighted acquisition also with a 1 to 5 rating scale.
Results
B0 InhomogeneityAbsolute offset of B0 ranged from 51 Hz to 94 Hz with a mean absolute offset of 50 ± 14 Hz and from 34 Hz to 118 Hz with a mean absolute offset of 64 ± 24 Hz for the right and left breast respectively. B0 variation ranged from 37 Hz to 52 Hz with a mean variation of 49 ± 9 Hz and from 25 Hz to 73 Hz with a mean variation of 43 ±14 Hz for the right and left breast respectively. Representative B0 maps are shown in Figure 2.
Apparent Diffusion Coefficient
Mean ADCs adjacent to the heart were 2.03 ± 0.21 x 10-3 mm2/s, 2.1 ± 0.26 x 10-3 mm2/s, 2.08 ± 0.24 x 10-3 mm2/s, and 2.08 ± 0.22 x 10-3 mm2/s for FB 2-shot, FB 4-shot, RG 2-shot and RG 4-shot respectively. Mean ADCs superior to the heart were 1.77 ± 0.23 x 10-3 mm2/s, 1.69 ± 0.52 x 10-3 mm2/s, 1.85 ± 0.13 x 10-3 mm2/s, and 1.8 ± 0.28 x 10-3 mm2/s for FB 2-shot, FB 4-shot, RG 2-shot and RG 4-shot respectively. The difference between 2-shot and 4-shot acquisitions (p = 0.697) and free-breathing and respiratory-gated acquisitions (p = 0.351) were not significant. ADCs adjacent to the heart were significantly higher than ADCs in slices superior to the heart (p < 0.001).
Observer Study
For sharpness, aliasing, perceived SNR and overall image quality there was a significantly higher proportion of ratings 4/5 for 4-shot versus 2-shot acquisitions (p = 0.003). and for respiratory-gating versus free-breathing (p < 0.001) (Figure 3). Inter-observer agreement for sharpness, aliasing, perceived SNR and overall image quality was 0.81 (0.76-0.87), 0.84 (0.78-0.89), 0.54 (0.38-0.71), and 0.78 (0.69-0.86) for free-breathing and 0.83 (0.77-0.89), 0.73 (0.63-0.83), 0.87 (0.82-0.92), and 0.65 (0.54-0.75) for respiratory-gating. Multi-shot DWI images from representative cases in the study are shown in Figure 4. In the distortion assessment 4-shot acquisitions were rated as having minimal to no distortion more frequently than the 2-shot acquisitions under both FB and RG (Figure 5).
Discussion and Conclusion
This work validates the robust performance of multi-shot DWI of the breast in the supine position and substantiates the potential for supine DWI to provide a non-invasive, comfortable and efficient breast cancer screening exam. The performance with respect to the level of aliasing is notable as strong aliasing would indicate failure of the multi-shot diffusion reconstruction. Further, the increased sharpness and reduced distortion resulting from an increased number of shots is achieved under both free breathing and respiratory gating. B0 inhomogeneity and ADC measurements provide starting points for characterization of the supine breast DWI imaging environment. The significant difference between ADC adjacent and superior to the heart may indicate an impact of cardiac artifacts.Acknowledgements
We gratefully acknowledge the research support of GE Healthcare and the following funding sources: NIH/NIBIB R01 EB009055 and NIH/NCI R01 CA249893.References
1. Gombos EC, Jayender J, Richman DM, et al. Intraoperative Supine Breast MR Imaging to Quantify Tumor Deformation and Detection of Residual Breast Cancer: Preliminary Results. Radiology. 2016;281:720-729.
2. Mallory MA, Sagara Y, Aydogan F, et al. Feasibility of Intraoperative Breast MRI and the Role of Prone Versus Supine Positioning in Surgical Planning for Breast-Conserving Surgery. Breast J. 2017;23:713-717.
3. Amornsiripanitch N, Bickelhaupt S, Shin HJ, et al. Diffusion-weighted MRI for Unenhanced Breast Cancer Screening. Radiology. 2019;293:504-520.
4. Baxter GC, Patterson AJ, Woitek R, Allajbeu I, Graves MJ, Gilbert F. Improving the image quality of DWI in breast cancer: comparison of multi-shot DWI using multiplexed sensitivity encoding to conventional single-shot echo-planar imaging DWI. Br J Radiol. 2021;94:20200427.
5. Naranjo ID, Lo Gullo R, Morris EA, et al. High-Spatial-Resolution Multishot Multiplexed Sensitivity-encoding Diffusion-weighted Imaging for Improved Quality of Breast Images and Differentiation of Breast Lesions: A Feasibility Study. Radiology: Imaging Cancer. 2020;2(3):e190076.
6. Chen NK, Guidon A, Chang HC, Song AW. A robust multi-shot scan strategy for high-resolution diffusion weighted MRI enabled by multiplexed sensitivity-encoding (MUSE). Neuroimage. 2013;72:41-47.
7. Reeder SB, Pineda AR, Wen Z, et al. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL): application with fast spin-echo imaging. Magn Reson Med. 2005;54:636-644.
8. Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61:29-48.
Figures
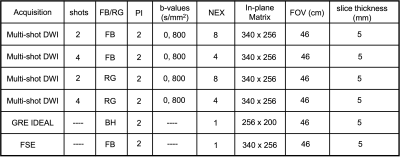
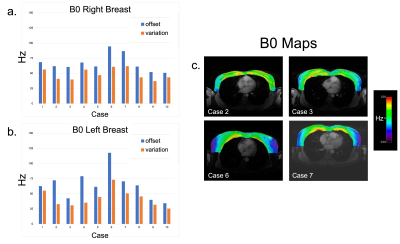
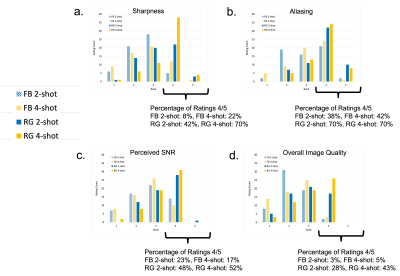
Figure 3. Cumulative ratings of all three radiologists for sharpness (a), aliasing (b), perceived SNR (c), and overall image quality (d), (rating 1: poorest performance, rating 5: highest performance). Percentage of ratings 4/5 for sharpness was highest with 4-shots and respiratory gating (a). Percentage of 4/5 ratings for aliasing increased with respiratory gating but did not vary between 2-shot and 4-shot with respiratory gating. Overall image quality had the lowest percentage of 4/5 ratings for all acquisitions (d) in comparison to the three other features.

Figure 4. Multi-shot diffusion-weighted images for two cases (case1: a-h, case 2: i-p) with varying degrees of motion demonstrate the lack of prominent aliasing artifacts in diffusion-weighted images (e-h, m-p) for all four acquisitions. Improvement in image sharpness achieved with an increased number of shots is evident in the diffusion-weighted images in the case with a less motion (e-h, solid arrows) while the improvement in image sharpness due to respiratory gating is more evident in the case with greater respiratory motion (m-n, dotted arrows).
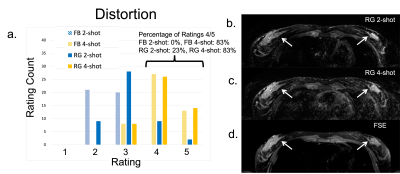
Figure 5. The 4-shot acquisitions (both FB and RG) were more frequently rated to have mild to no distortion (FB 4-shot: 83% 4/5, RG 4-shot 83% 4/5) versus the 2-shot acquisitions (FB 2-shot: 0% 4/5, RG 2-shot :23% 4/5) (a). In an example with respiratory gating (b-d) distortion in the 4-shot MUSE image (c, arrows) is reduced in comparison to the 2-shot image (b, arrows) and aligns more closely with tissue depiction in the undistorted FSE image (d, arrows).