3872
High-Resolution 3D-TOF MR Angiography in intracranial arteries and branches: A Initial Experience on Comparison between 3.0-T and 5.0-T1Zhongshan Hospital of Fudan University, Shanghai, China, 2Central Research Institute, United Imaging Healthcare, Shanghai, China
Synopsis
3D-Time-of-Flight MR Angiography (3D TOF-MRA) of the intracranial vessels is a first-line and noninvasive tool for the evaluation of patients with cerebrovascular disease. However, it is still challenged at 3.0-T MR imaging because peripheral segments of the main arteries can often not be sufficiently visualized. The expected remarkable increase in visualizations of intracranial arteries segments and vessel brancher provided by ultra-high field 5.0-T MRI may be valuable for addressing above issues. Our prospective analysis demonstrated that the 5.0-T TOF-MRA provides higher improvement in visualization of distal large arteries and small vessel branches than that at 3.0-T.
Introduction:
Three-dimensional time-of-flight magnetic resonance angiography (3D-TOF-MRA) based on 3.0 T MRI remains a first-line diagnostic tool and is able to provide a noninvasive assessment of cerebrovascular disease. However, it is still challenged at 3.0-T MRI imaging because peripheral segments of the main cerebral arteries can often not be sufficiently visualized. The expected remarkable increase in image quality provided by ultra-high field MRI may be valuable for addressing the above issues. Recently, the 5.0 T whole-body MRI imaging system was developed. Therefore, this study aims to evaluate the visualizations of intracranial arteries segments and vessel brancher with 5.0-T TOF-MRA. The purpose of our study was to evaluate the visualizations of intracranial arteries segments and vessel brancher with 5.0 T high-resolution 3D TOF-MRA.Methods:
Study Design: A prospective study was performed with 40 consecutive subjects (20 healthy volunteers and 20 patients with ischemic cerebrovascular events) who underwent either 3.0- or 5.0-T 3D-TOF-MRA in random order. The 5.0-T 3D-TOF-MRA was conducted with a whole-body MR imaging system (uMR Jupiter, United Imaging Healthcare,Shanghai, China). Images were independently graded by two radiologists on coronal, transverse, and sagittal maximum intensity projections according to diagnostic image quality, depiction of vessel segments, and the presence or absence of artifacts, both of whom were blinded to the acquisition technique and the field strength. Imaging score: The detailed scoring systems were as the followings [1]: 1) for image quality (from 1 to 5), 5=excellent (no artifacts present and all vessels in field of view depicted with same quality, which is close to that at digital subtraction angiography), and 1= non-diagnostic (image quality heavily impaired by artifacts and readers not able to assess vessels in field of view); 2) for visualization of vessel segments (from 0 to 3): 3=excellent depiction of vessel segment (small vessel segment clearly visualized and vessel-tissue contrast appears high), and 0=vessel segment not visible (small vessel segments not visualized); 3) for the artifacts: 5=absent, 4=minimal, 3= moderate, 2=interfering with image interpretation, 1=resulting in the non-diagnostic study. Statistical analysis: Mean values and SD were utilized for descriptive analysis of the continuous variables with normal distribution while median values and interquartile ranges (IQRs) were calculated for continuous variables with abnormal distribution. Continuous variables were compared between characteristics derived from 3.0T and 5.0T using the independent t test or Mann-Whitney U test. The reproducibility of scoring by two readers was evaluated using the intraclass coefficient (ICC) with a two-way random-effects model.Results:
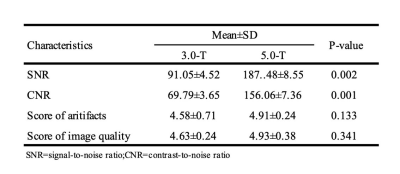
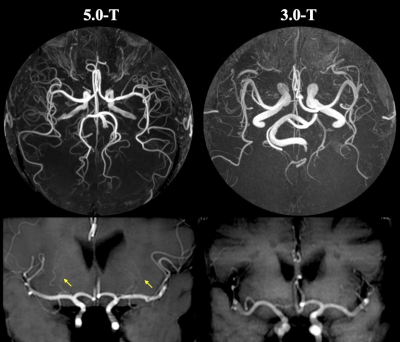
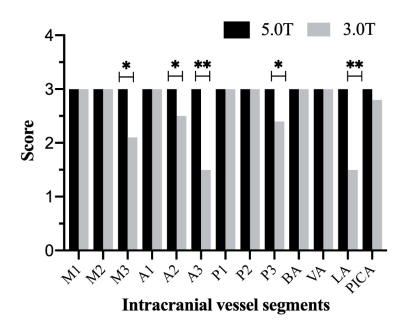
Interobserver agreements in the scoring of image quality and presence or absence of artifacts were excellent for both 3.0-T imaging and 5.0-T imaging, respectively, with ICC values of 0.93 for grading of image quality and 0.98 for grading of artifacts. Both 3.0-T and 5.0-T images were scored to provide the great image quality (mean score, 4.63±0.24 vs. 4.93±0.38; P=0.341) and fewest artifacts (mean score, 4.58±0.71 vs. 4.91±0.24; P=0.133). (Figure-1) Of the 220 vessel segments that were available for evaluation (11 segments in each subject or patient), 218 segments (99.6%) were visible at high-resolution 5.0-T imaging compared with 197 (89.5%) at standard 3.0-T imaging. As Figure-1 shown, the visualizations of distal large arteries including M3, A2/3 and P3 segments in 5.0-T TOF-MRA were significantly better than those in 3.0-T imaging (all P <0.05). Additionally, at 5.0-T imaging, depiction of small vessel branches especially in lenticulostriate arteries (LA) (Figure-2) was rated significantly higher than that at 3.0-T imaging [median (IQR), 3.0 (3.0, 3.0) vs 1.5 (1.0,3.1); P <0.001] (Figure-3). In all cases, signal intensity was significantly higher on 5.0-T TOF-MRA than that on 3.0-T images (P <0.001), and differences in SNR and CNR between 3.0-T imaging and 5.0-T imaging (91.05±4.52 vs 187.48±8.55, P =0.002), as well as CNR between 3.0-T imaging and 5.0-T imaging (69.79±3.65 vs 156.06±7.36, P =0.001), were statistically significant (Figure-1).Discussion:
3D TOF-MRA of the intracranial vessels is a reliable method and is able to provide noninvasive detection and evaluation of patients with cerebrovascular disease.[2] High-resolution 3D TOF-MRA is still limited at 3.0 T, however, peripheral segments of the main cerebral arteries, which are potential causes of infarction or potential locations of intracranial aneurysms, can often not be sufficiently visualized. To prove this, we performed an intraindividual comparative study to evaluate the added value of 5.0 T 3D TOF MRA. And the findings in our initial study demonstrated that the higher spatial resolution allowed better visualization of small vessel segments.Conclusion:
Intracranial high-resolution TOF-MRA at 5.0-T imaging provides higher improvement in visualization of distal large arteries and small vessel branches than that at 3.0-T imaging, which would be useful and helpful for accurate evaluation of cerebrovascular disease.Acknowledgements
NoneReferences
[1] Willinek WA, et al. Radiology. 2003;229(3):913-920.
[2] Mattern H, S, et al. Magn Reson Med. 2018;80(1):248-258.
Figures