3826
MR radiomic predictors of post-GKRS edema in meningiomas1Department of Biomedical Imaging and Radiological Sciences, National Yang Ming Chiao Tung University, Taipei, Taiwan, 2Department of Neurosurgery, Neurological Institute, Taipei Veteran General Hospital, Taipei, Taiwan, 3School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan, 4Department of Radiology, Taipei Veteran General Hospital, Taipei, Taiwan
Synopsis
Several issues concerning the optimal parameters of radiosurgery treatment, the occurrence of radiation-induced edema, and other postoperative complications remain unsolved in treating meningiomas. We aimed to determine whether combining radiomic features with clinical risk factors can improve the prediction of edema occurrence after Gamma-Knife radiosurgery (GKRS). Pre-GKRS MR radiomic features and clinical features were used to construct the prediction model. The model combing radiomic features and clinical features showed the highest performance for prediction of post-GKRS edema (AUC=0.79). The outcomes of this study can provide a risk assessment to facilitate precision medicine in treating meningiomas.
Background and Purpose
Meningioma is the most common intracranial tumor in adults, accounting for 33.8% of central nervous tumors. Nowadays, surgery and radiation therapy are the main treatment modalities for meningioma patients. Although Gamma-Knife radiosurgery (GKRS) has a good tumor control rate, some patients may have adverse radiation effects after GKRS, causing the reaction of surrounding tissues 1. Radiation-induced edema occurs principally within 1 to 24 months in 5% to 43% of patients after GKRS 2. In previous studies, factors that may contribute to postoperative edema, such as age, preoperative tumor, tumor size, tumor location, and treatment radiation dose, were considered as predictors of adverse radiation reactions after surgery 3. The purpose of this study was to establish a model that combines clinical indicators and quantitative MR radiomic features to predict the post-GKRS edema. We anticipate the inclusion of MR imaging biomarkers for predicting post-GKRS edema may further facilitate clinical decision-making in patients with meningioma.Materials and Methods
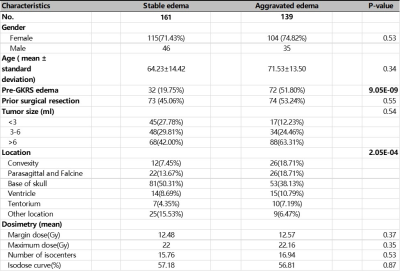
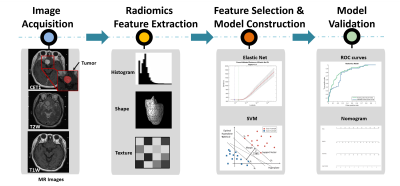
We enrolled 300 patients diagnosed with meningiomas at Taipei Veterans General Hospital. The inclusion criteria were as follows: 1) meningioma patients underwent GKRS treatment; 2) available information of postoperative edema; 3) complete data including pre-GKRS brain MRI examination and clinical factors (Table 1). All patients underwent brain T1-weignted imaging (T1W, TR/TE=500/9 ms), T2-weighted imaging (T2W, TR/TE=4000/109 ms), and contrast-enhanced T1W (CET1, TR/TE=500/9 ms) on a GE Medical Systems 1.5T magnetic resonance scanner before radiosurgery. Slice thickness was between 2.9 and 3.1 mm.Ten preoperative clinical features from these patients were collected: gender, age, pre-GK edema, prior surgical resection, tumor size (<3, 3-6, >6 ml), tumor location (convexity, parasagittal and falcine, base of skull or others), margin dose, maximum dose, number of isocenters, and isodose curve. We further extracted the three-dimensional radiomic features from the regions of interest (ROI) of tumors on the pre-GKRS MR images. A total of 1764 quantitative image feature parameters were extracted, including histogram, shape and size, and texture analysis 4.
In order to filter out non-significant features and prevent overfitting, two-sample t-test and elastic net algorithm were used to identify the radiomic features with significant differences between the postoperative aggravated edema and stable edema groups (p<0.05). The elastic net algorithm overcomes the limitations of the least absolute shrinkage and selection operator (LASSO) algorithm and improves the prediction performances 5. Three prediction models were built based on the clinical features, radiomic features, and combined features (both clinical and radiomic features), respectively. The receiver operating characteristic (ROC) curve and nomogram were displayed to evaluate the model performance. A flowchart of this study is shown in Figure 1.
Results and Discussion
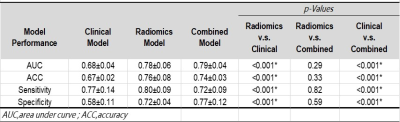
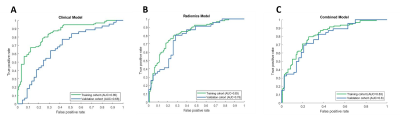
As shown in Table 1, pre-GKRS edema and tumor location showed significant relationships with postoperative edema (p <0.05). Conversely, we found no significant differences in gender, age, and dosimetry features (including margin dose, maximum dose, number of isocenters, and isodose) between the postoperative aggravated edema and stable edema groups (p = 0.34 to 0.87). Three preoperative clinical features including age, pre-GKRS edema, and tumor size were used to build a clinical model based on logistic regression analysis. The performance in predicting post-GKRS edema based on the clinical model could achieve AUC=0.85 in the training set and AUC=0.68 in the validation set. (Figure 2A)For the radiomic model, we first screened 1762 radiomic features by the two-sample t-test. Secondly, we used the elastic net algorithm to identify 19 key features for the subsequent model training. Six features were from CET1, four features were from T2W, and nine features were from T1W. In addition, texture features accounted for two-thirds of these key features (n=13), while histogram features accounted for one-third (n=6). Finally, the support vector machine (SVM) regression model was used to predict the post-GKRS edema.[6] The radiomic model achieved an AUC for the prediction of post-GKRS edema of 0.83 in the training set and 0.78 in the validation set. (Figure 2B)
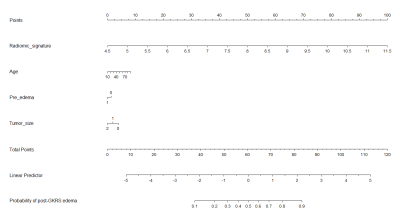
We further combined the key clinical and radiomic features (including three clinical characteristics and nineteen radiomics features) to construct a combined model. For the training set, the prediction performance of the combined model showed an AUC of 0.83 with a sensitivity of 83.3%, specificity of 75.8%. For the validation set, the combined model showed an AUC of 0.79 with a sensitivity of 72.3%, specificity of 77.1%. (Figure 2C) Also, the combined model is presented as a nomogram in Figure 3.
Among these three models, the performance of combined model was equivalent to the radiomic model (p = 0.29). Nevertheless, the combined model and the radiomic model were both significantly outperformed the clinical model in predicting post-GKRS edema. The detailed performance for three constructed models is shown in Table 2.
Conclusions
In this retrospective study, we reported that the combined model using key radiomic and clinical features can help predict post-GKRS edema in patients with meningioma. It can predict whether the patient may suffer from the radiation-induced edema and therefore assist the individualized adjustment to reach optimal treatment setup.Acknowledgements
This study was supported by Ministry of Science and Technology of Taiwan (109-2314-B-010-022-MY3), Taipei Veterans General Hospital, National Yang Ming Chiao Tung University, and University System of Taiwan (VGHUST110-G7-2-2).References
1. Wiemels, J., M. Wrensch, and E.B. Claus, Epidemiology and etiology of meningioma. Journal of Neuro-Oncology, 2010. 99(3): p. 307-314.
2. Milano, M.T., et al., Radiation-Induced Edema After Single-Fraction or Multifraction Stereotactic Radiosurgery for Meningioma: A Critical Review. Int J Radiat Oncol Biol Phys, 2018. 101(2): p. 344-357. 3. Patil, C.G., et al., Predictors of peritumoral edema after stereotactic radiosurgery of supratentorial meningiomas. Neurosurgery, 2008. 63(3): p. 435-40; discussion 440-2.
4. Lu, C.F., et al., Machine Learning-Based Radiomics for Molecular Subtyping of Gliomas. Clin Cancer Res, 2018. 24(18): p. 4429-4436.
5. Kayanan, M. and P. Wijekoon, Performance of LASSO and Elastic net estimators in Misspecified Linear Regression Model. 2019. 48: p. 293. 6. Xiao, B., et al., Three-Dimensional Radiomics Features From Multi-Parameter MRI Combined With Clinical Characteristics Predict Postoperative Cerebral Edema Exacerbation in Patients With Meningioma. Front Oncol, 2021. 11: p. 625220.
Figures