3812
Systematic investigation of gamma knife in the treatment of brain tumors: an MR perfusion imaging study
ling huang1, hui bai1, HAI ZHONG1, and WEI QIANG DOU2
1the second hospital of shandong university, JINAN, China, 2GE Healthcare, MR Research, BEIJING, China
1the second hospital of shandong university, JINAN, China, 2GE Healthcare, MR Research, BEIJING, China
Synopsis
The main purpose was to evaluate the gamma knife radiosurgery(GKRS) treatment effect of multiple kinds of brain tumors by MR perfusion imaging. We collected 45 patients with three kinds of brain tumors treated with GKRS. Perfusion imaging, including 3D-ASL and DSC-PWI, was performed before and after treatment. ASL-rCBF, DSC-rCBF and DSC-rCBV decreased significantly after GKRS treatment, and ASL-rCBF before GKRS treatment showed the most robust performance with high AUC in predicting GKRS treatment effect. With these findings, MR perfusion imaging can be considered a time and effective method understanding the treatment effect of GKRS for brain tumor patients.
Introduction
Gamma knife radiosurgery (GKRS) has been considered by neurosurgeons an effective method for brain tumor patients with intrinsic features of light injury and good tolerance [1-2]. Moreover, this method does not affect the survival time and can be clinically repeated in multiple times. Although promising effect of treatment can usually be achieved, However, no gold standard has been well recognized to evaluate its treatment effect for brain tumor patients so far.MR perfusion imaging, as a well-established method, can measure accurate blood flow quantitatively. In general, two main kinds of perfusion imaging, including dynamic -susceptibility-contrast perfusion-weighted-imaging (DSC-PWI) with contrast agent required and 3D pseudo-continuous arterial-spin-labeling (3D-pcASL) without contrast agent injection, have been widely applied in clinic[3]. A number of studies have applied either of these two techniques in grading tumor or evaluating treatment response. With these promising results, we assumed that combined both DSF-PWI[4] and 3D-pcASL[5] might have clinical potential in evaluating the treatment effect of GKRS. However, no such study has been explored so far. Therefore, this work aimed to comprehensively evaluate the treatment effect of GKRS on multiple kinds of brain tumors by combing 3D-ASL and DSC-PWI.Materials and methods
45 brain tumor patients, including 34 brain metastases (75.6%), 5 meningiomas (11.1%) and 6 vascular malformations (13.3%) were retrospectively recruited in this study. Each patient underwent GKRS treatment and perfusion imaging before and after treatment. All MRI examinations were performed on a 3T MRI scanner (discovery750, GE Healthcare) with 8-CH head and neck unit coil. MRI scan protocol included conventional brain imaging (T2WI, T1WI, T2 FLAIR), diffusion weighted imaging, 3D-pcASL, DSC-PWI and 3D T1w high-resolution anatomic imaging. For 3D-pcASL imaging, the scanning parameters were set as TR=4632ms, TE=10.5ms, bandwidth=62.5kHz, NEX=3, number of arms=8, points per arm=512, slice thickness=4mm, post-label-delay (PLD)= 2025ms. DSC-PWI was obtained using echo-planar-imaging (EPI) gradient-echo sequence (TR=1500ms, TE=15ms, flip angle=90degree, bandwidth=250kHz, slice thickness=5mm, time resolution=1.5s). In DSC imaging, an intravenous injection of gadolinium contrast was used at dose of 0.2 mmol / kg and a rate of 4.0 ml / s. 3D-pcASL and DSC-PWI data were post-processed in vendor-provided software on GE Medical System workstation (ADW 4.6). The corresponding ASL derived CBF maps and DSC derived rCBF, DSC-rCBV, DSC-MTT and DSC-TTP maps were obtained for each patient. In addition, T1w high-resolution anatomic images were analyzed in gamma plan system (Elekta, Stockholm, Sweden) to obtain tumor volume for each patient.Two radiologists were employed to manually draw regions of interest (ROI)s on tumors and the contralateral sides on 3D T1w high-resolution anatomic images, and fused each ROI on ASL-CBF maps correspondingly. DSC-PWI adopted AIF mode (brainstat AIF). Identical measurement method was applied to obtain DSC-rCBF, DSC-rCBV, DSC-MTT and DSC-TTP for each tumor.All statistic analyses were performed using IBM SPSS Statistics version20.0. Inter-observer agreement for perfusion parameter measurements over two radiologists was assessed with intraclass correlation coefficient (ICC). ICC value of greater than 0.75 was considered good reproducibility. Paired-samples t-test or Wilcoxon signed ranks test was used to compare the volume changes of tumor before and after operation. The difference of ASL-rCBF, DSC-rCBF, DSC-rCBV, DSC-MTT, and DSC-TTP between pre- and post-operation were analyzed by Wilcoxon signed ranks test. Each two of these parameters were also performed with correlation analysis with Pearson’s correlation analysis. Receiver operating characteristic (ROC) analysis was also separately applied to test the efficacy of ASL-rCBF, DSC-rCBF or DSC-rCBV before GKRS . P < 0.05 was considered statistically significant.Results
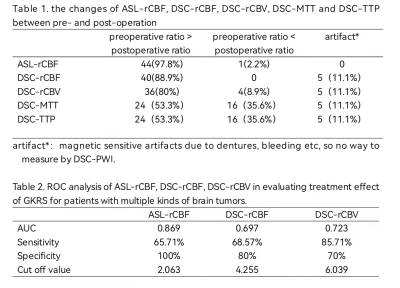
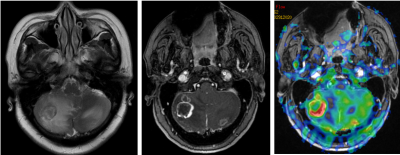
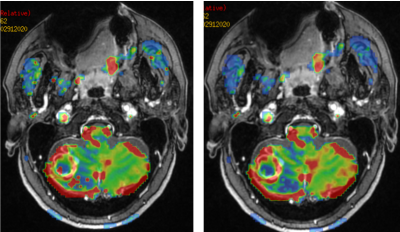
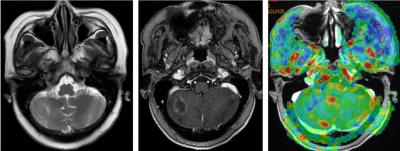
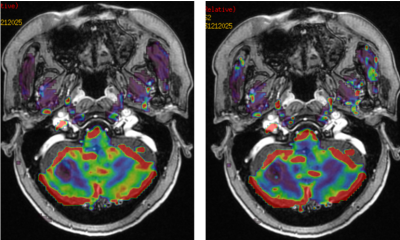
The interobserver agreement of ASL and DSC-PWI parameter measurements was excellent with high ICCs of 0.989 and 0.946, respectively. Using GKRS, the tumor volume was significantly reduced post-operatively than pre-operatively (P<0.001). Significantly different ASL-rCBF, DSC-rCBF and DSC-rCBV were observed between pre- and post-operation (all P<0.001) (figure1-4), while comparable values were found in DSC-MTT and DSC-TTP (P>0.05;Table.1). Pearson’s correlation analysis showed a significantly positive correlation between ASL-rCBF and DSC-rCBF (r=0.825, p<0.001), and ASL-rCBF and DSC-rCBV (r=0.625, p<0.001) pre-and postoperation. With ROC analysis, robust efficacies of ASL-rCBF, DSC- rCBF and DSC-rCBV with high AUCs of 0.869, 0.697 and 0.723 were found in assessing the treatment effect of GKRS The corresponding sensitivity, specificity and cut-off values were also shown (Table.2).Discussion and conclusion
This study mainly investigated the feasibility of MR perfusion imaging of 3D-pcASL and DSC-PWI in evaluating the treatment effect of gamma knife on multiple kinds of brain tumors. After GKRS, significantly decreased ASL-rCBF, DSC-rCBF and DSC-rCBV were observed for all patients with different types of brain tumors, even if the tumor volumes didn’t have apparent change. This finding indicates that no new capillary formed and vasodilated in tumor, or the activity of tumor cells decreased after GKRS treatment. In addition, with high AUC, robust efficacies of both 3D-pcASL and DSC-PWI were confirmed in assessing treatment effect of GKRS.In conclusion, combined 3D-pcASL and DSC-PWI can reflect sensitively the physiological and pathological changes of tumors after GKRS, and can thus be considered effective methods in evaluating the therapeutic effect of gamma knife for brain tumor patients.Acknowledgements
No acknowledgement found.References
1. Paris J, Angeli E, Bousquet G. The Pharmacology of Xenobiotics after intracerebro Spinal Fluid Administration: Implications for the Treatment of Brain Tumors. Int J Mol Sci.2021 Jan 28 ;22(3).2. Suh JH, Kotecha R, Chao ST, Ahluwalia MS, Sahgal A, Chang EL. Current approaches to the management of brain metastases. Nat Rev Clin Oncol.2020V17N5:279-299.3. GAO Xiao, ZHANG Xue-ning, ZHANG Yun-ting, YU Chun-shui and XU De-sheng. Magnetic resonance imaging in assessment of treatment response of gamma knife for brain tumors. Chin Med J 2011;124(12):1906-1910.4. Nader Zakhari, MD, Michael S. Taccone, Carlos H. Torres, Santanu Chakraborty, John Sinclair, et al. Prospective Comparative Diagnostic Accuracy Evaluation of Dynamic Contrast-Enhanced (DCE) vs. Dynamic Susceptibility Contrast (DSC) MR Perfusion in Differentiating Tumor Recurrence From Radiation Necrosis in Treated High-Grade Gliomas. J. MAGN. RESON. IMAGING 2019: 1-10. Volodia Dangouloff-Ros, Christophe Deroulers, Frantz Foissac, Mathilde Badoual, Eimad Shotar, David Grévent, Raphael Calmon, et al. arterial spin labeling to Predict Brain Tumor grading in children: Correlations between Histopathologic Vascular Density and Perfusion MR Imaging. Radiology: Volume 281: Number 2—November 2016.
DOI: https://doi.org/10.58530/2022/3812