3810
Identification and diagnosis of hepatocellular carcinoma in high-risk patients with an abbreviated-protocol MR screening: a pilot study1Radiology, West China Hospital, Sichuan University, Cheng Du, China, 2GE Healthcare Beijing China, Beijing, China, 3West China Hospital, Sichuan University, Cheng Du, China
Synopsis
Early detection and diagnosis of hepatocellular carcinoma (HCC) is essential for patients’ prognosis, however, the imaging hallmarks for tumor detection and diagnosis has remained same for years despite the use of many new imaging methods. Thus, in this study, we aimed to prospectively evaluated the detection performance of various MR sequences and abbreviated MRI (aMRI) protocols in different clinical settings and further compared the different imaging criteria for the diagnosis of HCC using either extracellular contrast agent (ECA) or hepatobiliary specific contrast (HBSC) MR imaging, and the developed diagnostic criteria for detection and diagnosis of HCC may aid clinical diagnosis.
Introduction
Early detection and diagnosis of hepatocellular carcinoma (HCC) in high-risk patients plays a vital role in clinical practice, especially for patients’ long-term prognosis1,2. At present, the multiparametric liver MR imaging has been designed and applied for the evaluation of the hepatic tumor3,4. However, the long scanning time and high-cost effectiveness of these protocols limit their regular use in clinical practice. Recently, it has been reported that the emerging abbreviated MRI (aMRI) protocols of liver may have potential to overcome these limitations and further increase the availability of this imaging test5-6. However, of those studies, the nodules size was not strictly restricted (<3 cm) which may potentially increase the screening performance5, and there is still little known about the screening performance of aMRI protocol in non- hepatobiliary specific contrast (HBSC) group. Therefore, the purpose of this study was to prospectively evaluate the detection performance of hepatic nodules in high-risk patients, and then to further determine the lesion characterization ability of each aMRI protocol in detecting the clinically significant HCC in patients underwent either extracellular contrast agent (ECA) or HBSC group, in comparison with the conventional imaging hallmark and using the histopathological results as reference standard.Methods
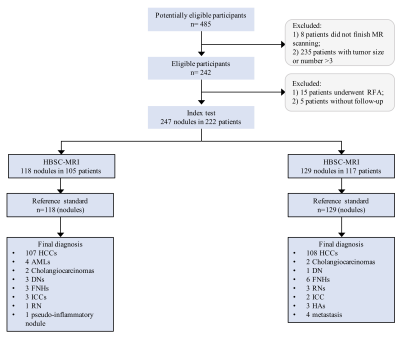
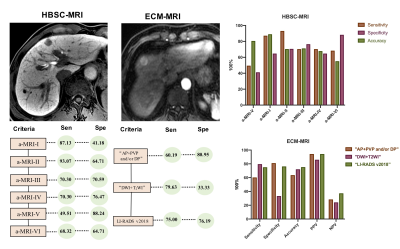
This study was approved by the institutional review board and the written informed consent was obtained from all patients. This prospective study included 247 nodules in 222 patients (mean age, 53.32 ±10.84 years; range, 22-79 years) from January 2017 and June 2020. Detailed information about the inclusion criteria were shown in Figure 1. Patients were categorized as HBSC and ECA group according to the use of contrast agent. MR imaging was carried out using 3.0 T MR systems (Discovery 750w, GE Healthcare, Milwaukee, USA; Skyra 3.0 T, Siemens Healthcare, Erlangen, Germany). Sixteen-channel phased-array torsor coils were used for all measurements. The standard liver MR protocols were applied. According to the detection performance, different MR sequences were combined as aMRI protocols in different clinical settings. In this study, for the HBSC-MRI group, five aMRI protocols were created including: 1) a-MRI-I: diffusion weighted imaging (DWI) + T2WI; 2) a-MRI-II: DWI + hepatobiliary phase (HBP); 3) a-MRI-III: arterial phase (AP) + portal venous phase (PVP)and/or TP+ and/or HBP (Korean Guidelines 2018)7; 4) a-MRI-IV: AP+PVP and/or+HBP (Japan Society of Hepatology Guideline 2014)8; 5) a-MRI-V: AP+PVP only (European Association for the Study of the Liver (EASL))9; 6) a-MRI-VI: The Liver Imaging Reporting And Data System 2018 (LI-RADS v2018), and when the nodule was assessed as LI-RADS 4 or 5, the nodule was finally determined as HCC with the LI-RADS criteria. In addition, for the ECA-MRI group, three protocols including the conventional imaging hallmark of “AP+PVP and/or DP”, “DWI + T2WI”and LI-RADS v2018 were created. Of these aMRI protocols, the detection performance was calculated and the best aMRI protocol in different clinical settings was determined. Furthermore, for each aMRI protocol and clinical guidelines, only these positive imaging features were presented, and the lesion can be characterized as HCC lesion. Unless, the hepatic nodule should be determined as non-HCC. The detection performance and imaging features of each nodule were evaluated in all MR sequences by three experienced abdominal radiologists. Detection performance of each nodule on all MR sequences were compared and further the diagnostic performance of various diagnostic criteria were evaluated.Results
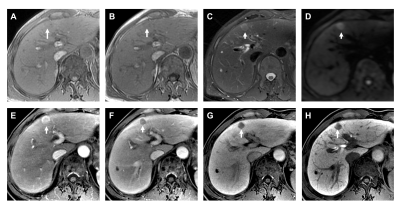
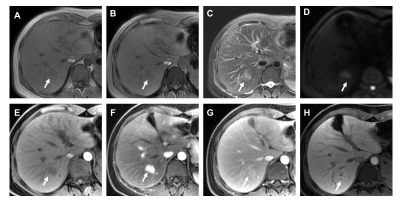
In total, there were 247 nodules (mean size, 17.65 ±6.76 mm, range, 4-30 mm) were analyzed in 222 patients, which consisted of 209 HCCs (Figure 2) and 38 non-HCC nodules, such as focal nodular hyperplasia(FNH)(Figure 3), all these hepatic nodules were confirmed by histopathological results. For those patients who underwent ECA-MRI, the conventional imaging hallmark of “AP+PVP and/or DP” was recommended, as 100% lesion detection rate and 60.19% sensitivity and 80.95% specificity. Additionally, for those patients who underwent HBSC-MRI, the diagnostic criteria of “DWI+HBP” was strongly recommended (Figure 4). This diagnostic criteria demonstrated, both in all tumor size and for nodules ≤2 cm, higher sensitivity (93.07% and 90.16%, all p<0.05, respectively) and slightly lower specificity (64.71% and 87.50%, all p>0.05, respectively) than that of EASL criteria.Discussion
The results of our study indicated that for patients with HBSC-MRI, our new diagnostic criteria, based on the evaluation of HBP and DWI, demonstrated a higher lesion detection rate, and a significantly higher diagnostic sensitivity compared with that of EASL and Asian guidelines and a specificity slightly but not significantly lower than that of EASL and Asian guidelines for HCC, which were in line with Kim HD et al10, that means, by using new diagnostic criteria may enable more detection and characterization of early HCC and thus further improve the prognostic performance. Our study also found that for patients with ECA-MRI, the conventional diagnostic hallmark showed the highest detection and diagnostic performance, suggesting that the application of diagnostic criteria for HCC need to be differentiated in patients using HBSC-MRI and those with ECA-MRI.Conclusions
Different diagnostic criteria were recommended according to the lesion detection and diagnostic performance in different clinical settings. Our new diagnostic criteria demonstrated high lesion detection rate and significantly higher sensitivity, comparable specificity than that of EASL criteria for HCC with HBSC-MR.Acknowledgements
No acknowledgement found.References
1. An C, Kim DW, Park YN, Chung YE, Rhee H, Kim MJ. Single Hepatocellular Carcinoma: Preoperative MR Imaging to Predict Early Recurrence after Curative Resection. Radiology 2015;276:433-443.
2. Lee S, Kim SH, Lee JE, Sinn DH, Park CK. Preoperative gadoxetic acid-enhanced MRI for predicting microvascular invasion in patients with single hepatocellular carcinoma. Journal of hepatology 2017;67:526-534.
3. Canellas R, Patel MJ, Agarwal S, Sahani DV. Lesion detection performance of an abbreviated gadoxetic acid-enhanced MRI protocol for colorectal liver metastasis surveillance. European radiology 2019;29:5852-5860.
4. Canellas R, Rosenkrantz AB, Taouli B, Sala E, Saini S, Pedrosa I, et al. Abbreviated MRI Protocols for the Abdomen. Radiographics : a review publication of the Radiological Society of North America, Inc 2019;39:744-758.
5. Lee JY, Huo EJ, Weinstein S, Santos C, Monto A, Corvera CU, et al. Evaluation of an abbreviated screening MRI protocol for patients at risk for hepatocellular carcinoma. Abdominal radiology (New York) 2018;43:1627-1633.
6. Marks RM, Ryan A, Heba ER, Tang A, Wolfson TJ, Gamst AC, et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR American journal of roentgenology 2015;204:527-535.
7. 2018 Korean Liver Cancer Association-National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma. Korean journal of radiology 2019;20:1042-1113.
8. Kudo M, Matsui O, Izumi N, Iijima H, Kadoya M, Imai Y. Surveillance and diagnostic algorithm for hepatocellular carcinoma proposed by the Liver Cancer Study Group of Japan: 2014 update. Oncology 2014;87 Suppl 1:7-21.
9. Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology (Baltimore, Md) 2014;60:715-735. 10. Kim HD, Lim YS, Han S, An J, Kim GA, Kim SY, et al. Evaluation of early-stage hepatocellular carcinoma by magnetic resonance imaging with gadoxetic acid detects additional lesions and increases overall survival. Gastroenterology 2015;148:1371-1382.
Figures