3771
High-resolution DWI for liver lesion detection in patient at-risk for HCC: prospective comparison with the HBP using gadoxetic acid1Department of Radiology, West China Hospital, Chengdu, China, 2Clinical Science, Philips Healthcare, Cheng du, China
Synopsis
Compared with conventional diffusion-weighted imaging (DWI), high-resolution DWI (HR-DWI) can improve the image quality with higher image scores. In patients with increased risk for hepatocellular carcinoma, gadoxetic acid-enhanced MRI with HR-DWI showed comparable performance with conventional DWI + hepatobiliary phase for detecting potentially malignant liver lesions.
Introduction
Hepatobiliary phase (HBP) of gadoxetic acid-enhanced MR imaging has been playing a pivotal role in the diagnosis and staging of in hepatocellular carcinoma (HCC) given superior sensitivity for detecting minute liver lesions [1, 2]. However, it comes at the cost of decreased specificity, suboptimal acquisition of the arterial phase images, increased motion artifacts, and prolonged scanning time [3]. Diffusion-weighted imaging (DWI) is a potential surrogate MR technique to HBP in this setting. Previous reports have demonstrated the incremental diagnostic values of DWI to standard MRI for HCC, particularly in improving sensitivity with acceptable specificity [4]. However, conventional DWI frequently suffers from geometric distortion and low spatial resolution. In contrast, high-resolution DWI (HR-DWI) has emerged as a new DWI technique which showed promise to improve spatial resolution, reduce distortion, and optimize signal-to-noise (SNR) compared with conventional parallel imaging-based method.Therefore, in patients at increased risk for HCC, this prospective study aimed to 1) compare the image quality of HR-DWI with conventional DWI as well as to 2) evaluate the ability of gadoxetic acid-enhanced MRI with HR-DWI against conventional DWI with HBP for detecting potentially malignant hepatic lesions.
Methods
Our institutional review board approved this single-center prospective study, and written informed consent was obtained from each participant. Between September 2020 and October 2021, consecutive patients at high risk for HCC with focal liver lesions were enrolled. All patients underwent gadoxetic acid-enhanced MRI on a 3-T system with a 32-channel phased-array coil (Ingenia Elition 3.0T; Philips Healthcare, Best, The Netherlands). The standard liver MRI protocol included: 1) T2-weighted imaging; 2) conventional DWI (b values:0, 200 and 1000 s/mm2) with apparent diffusion coefficient (ADC) maps; 3) HR-DWI with ADC maps; and 4) dynamic T1-weighted imaging before and after injection of gadoxetic acid in the late arterial phase, portal venous phase, transitional phase, and the HBP. HR-DWI images were obtained with the following acquisition parameters: FOV = 512×512mm2, TR/TE = 2775/74 ms, slice thickness= 6 mm, imaging matrix =344×249, bandwidth = 1457Hz/Px, flip angle=90, and acquisition time (TA) = 400s.All MR images were independently reviewed by two fellowship-trained abdominal radiologists (with 5, and 11 years of experience in liver MRI, respectively). Two sets of MR images were evaluated: 1) dynamic contrast-enhanced images (without HBP images) + HR-DWI (termed the “HR-DWI group”); and 2) dynamic contrast-enhanced images + conventional DWI + HBP (termed the “conventional DWI + HBP group”). Subjective image quality was assessed using a 5-point Likert scale (1 = poor, 5 = excellent) for image anatomic distortion, lesion conspicuity, detail structure, and the overall image quality. Number and size of LR-3/4/5/M lesions based on the Liver Imaging Reporting and Data System (LI-RADS) version 2018 were documented [5]. In patients with LR-5 (definite HCC) lesions, the Barcelona Clinic Liver Cancer (BCLC) stages were evaluated. The Likert scales and quantitative parameters (lesion number and size) were compared using the Wilcoxon signed-rank test and paired t-test. Intra-class correlation coefficient (ICC) were used for BCLC staging. Two-tailed P < 0.05 was considered statistically significant.
Results
A total of 29 high-risk patients (mean/medium age: 65/57 years; men/women: 25/4) were included during the study period. HR-DWI showed significantly higher image quality score than conventional DWI (4.52±0.58 vs 3.48±0.86, P < 0.001). A total of 121 LR-3/4/5/M lesions (mean size: 1.92±2.158) were detected in the HR-DWI group, while 167 LR-3/4/5/M lesions (mean size: 1.60±2.478) were detected in the conventional DWI + HBP group. No difference in LR-3/4/5/M lesion number (P = 0.116) or size (P = 0.307) was detected between the two groups. In patients with LR-5 lesions (n = 18), there was excellent agreement for the BCLC staging between the two groups (ICC=0.935 95%CI [0.637-0.930]).Discussion
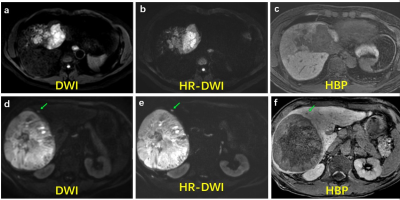
In the comparison of image quality, the performance of HR-DWI is better than that of traditional DWI. Figure 1 showed that the lesion is more conspicuous with a clear margin and less distortion on HR-DWI(Fig.1 b and e). These results indicate that HR-DWI has clinically applicable image quality, which is expected to improve the detection ability of liver tumors and evaluate the diagnostic performance of HCC diagnosis. Moreover, the results of our study showed that HR-DWI can achieve the high detection rate of liver lesions at high-risk comparable to that of conventional DWI with hepatobiliary phase, which may be used as a potential alternative to HBP (or even EOB-MRI) in the clinic.Conclusion
Our results indicate that HR-DWI showed ability for hepatic lesions detection compared with HBP in gadoxetic acid-enhanced MRI, which was reflected by an increased image quality, along with a higher confidence for liver tumor detection.Acknowledgements
No acknowledgement found.References
1. Ahn SS, Kim MJ, Lim JS, Hong HS, Chung YE, Choi JY (2010) Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology 255:459–466
2. Cha DI, Lee MW, Kim YK et al (2014) Assessing patients with hepatocellular carcinoma meeting the Milan criteria: is liver 3 tesla MR with gadoxetic acid necessary in addition to liver CT? J Magn Reson Imaging 39:842–852
3. Narita M, Hatano E, Arizono S et al (2009) Expression of OATP1B3 determines uptake of Gd-EOB-DTPA in hepatocellular carcinoma. J Gastroenterol 44:793–798
4. Piana G, Trinquart L, Meskine N, Barrau V, Beers BV, Vilgrain V (2011) New MR imaging criteria with a diffusion-weighted sequence for the diagnosis of hepatocellular carcinoma in chronic liver diseases. J Hepatol 55:126–132
5. Marrero JA, Kulik LM, Sirlin C, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018; 68(2):723–750.
Figures