3761
A clinicopathological-radiological nomogram for prognosis of postoperative hepatocellular carcinoma1Department of Radiology, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy, Guangzhou, China, 2Philips Healthcare, Guangzhou, China
Synopsis
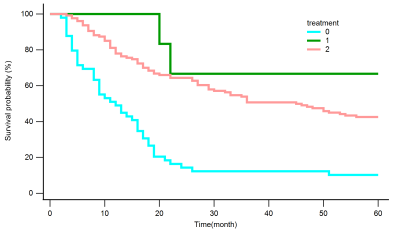
Few studies both focus on the prognosis for patients with early recurrence and five years overall survival (OS) for patients with BCLC 0-C. Here, we established nomograms for predicting 5-year overall survival and early recurrence after curative resection of Hepatocellular carcinoma (HCC) based on clinicopathological-radiological model and investigated whether different treatment methods have influenced on OS for patients with early recurrence. The results demonstrate that the nomogram, based on clinical, pathological and radiological factors, had good accuracy in estimating OS and recurrence respectively. Further, reoperation maybe the best option for patients with recurrence in good condition.
Background
HCC is ranked as the sixth most common neoplasm and the third leading cause of cancer-related death [1]. Surgical resection remains the firstline treatment and is regarded as a curative therapy for patients with resectable HCC. However, 50% to 70% of HCC patients experience recurrence after surgical resection within 5 years [2].Therefore, it is critical to find a robust method to more accurately predict early recurrence and postoperative survival to further improve the prognosis of HCC patients, which are helpful for both postoperative management and clinical decision-making in the treatment of HCC patients. To date, some significant models are built between preoperative imaging features and clinical characteristics [3]. However, most of them only focus on early stage or solitary HCC, lessly combining preoperative imaging features and postoperative pathological characteristics together. In addition, there are few studies both focusing on the prognosis for patients with early recurrence and five years overall survival, for one of which most of studies models only were built. Here, we aimed to identify preoperative MR imaging features, according to LI-RADS major and auxiliary features, clinical and postoperative pathological characteristics to establish nomograms for predicting 5-year OS and early recurrence (<2 years) after curative resection of HCC based on Random survival forest (RF) model model. This study also investigated whether different treatment methods have influenced on OS for patients with early recurrence.Materials and Methods
This retrospective study recruited 494 HCC patients (428 men and 66 women; mean age, 51.28 years ± 11.29; range,18–80 years) who underwent liver resection from January 2010 to December 2015. Clinical pathology, radiology and follow-up data were collected. MRI examination of each patient was performed using one of the three 3.0-T systems (GE Medical Systems; Siemens Medical Solutions; Philips Medical System) within 1 month before surgery. For temporally independent validation, patients who underwent surgery prior to April 2015 were assigned to a training cohort (n = 346), and the subsequent patients were assigned to a validation cohort (n = 148) at a ratio of 7:3. Random survival forest (RF) model were uesed for preoperative MR imaging features, clinical and postoperative pathological characteristics selection. Then, nomograms estimating OS and early recurrence were constructed using multivariate Cox regression analysis further. The discrimination and calibration abilities of the nomograms were evaluated by concordance indexes (C-index), calibration curves, and Kaplan-Meier curves. OS curves of different treatments for patients with early recurrence after surgery were depicted using the Kaplan–Meier method and compared using the log-rank test.Results
Nomogram of OS also was developed based on 7 prognostic factors (BCLC, nonsmooth margin, maximum tumor diameter, microvascular invasion, age, AST and differentiation) with good predictive performance in the training (C-index: 0.787, n=346) and validation cohorts (C-index: 0.711, n=148) (Figure 1). Nomogram of recurrence free survival also was developed based on 4 prognostic factors (BCLC, nonsmooth margin, maximum tumor diameter and microvascular invasion) with good predictive performance in the training (C-index: 0.717, n=346) and validation cohorts (C-index: 0.7, n=148) (Figure 2). In comparison to the BCLC staging system, the C-index (training cohort: 0.787vs. 0.678, 0.717 vs 0.675, n=346; validation cohort: 0.741 vs. 0.672, 0.701 vs 0.671, n=148, respectively for OS and RFS), and model’s calibration curves all showed improved performance. Patients who received surgery after tumor recurrence had higher retreated OS compared to comprehensive treatments and supportive care (Figure 3).Conclusion
Two nomograms combining clinicopathological and multiparametric MRI demonstrated good discriminative ability in predicting postoperative 5-year OS and early recurrence (≤2 year) for HCC respectively. For patients with recurrence HCC , the prognosis of continued surgical treatment may be better than non-surgical treatment.Acknowledgements
No acknowledgement found.References
1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
2. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723-50.
3. Ren Z, He S, Fan X, He F, Sang W, Bao Y, Ren W, Zhao J, Ji X, Wen H. Survival prediction model for postoperative hepatocellular carcinoma patients. Medicine (Baltimore). 2017 Sep;96(37):e7902.
Figures