3754
Brain Functional Connectome prospectively encodes Distress Symptoms During COVID-19 pandemic1Huaxi MR Research Center, Chengdu, China
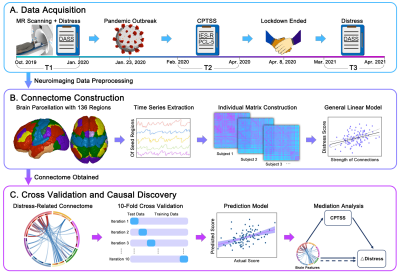
Synopsis
In the prospective investigation of public mental health following COVID-19 pandemic, we assessed the psychological status of a general sample. Furthermore, we built a brain-distress construct which mainly contained within- and between-DMN connection patterns, and the left hippocampus emerged as the hub region in distress-related connectome. Based on customized brain connectomes, we may identify individuals who confer high vulnerability to pandemic-induced distress symptoms with well-performing predictive modeling. Our findings may facilitate the understanding of neural correlates underlying distress on the individual macro-scale network level, and the susceptibility markers may serve as targets for prevention and intervention.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has generated a chronically constant state of tension with a surge of public mental health crises 1,2. Given the pervasive life events of uncertainty during pandemic, individuals may be increasingly vulnerable to psychological distress problems 3,4. Regarding great individual variations in pandemic-induced distress among the general public 5, exploring neuromarkers in marco-scale brain networks to identify those who are at high risk for developing persistent distress symptoms may facilitate addressing the salient mental health issues 6. Herein, we explore the changes of psychological distress following COVID-19 pandemic, and then build the altered brain construct that prospectively encodes the persistent distress symptoms.Material and Methods
A total of 100 healthy individuals were recruited for neuroimaging scanning and self-reported psychological scales from October 2019 to January 2020. All participants were recontacted for second-wave psychological evaluations including COVID-related questionnaires to assess symptoms during the initial outbreak and the peak from February to April 2020 and follow-up psychological scales to assess mental health from March to April 2021. The distress symptoms of participants were evaluated by the 21-item Depression Anxiety Stress Scales, and the COVID-related posttraumatic stress symptoms (CPTSS) were assessed by the Impact of Event Scale-Revised and the Posttraumatic Stress Disorder Checklist for DSM-5.The cerebral cortex was divided into seed regions according to a 100-area parcellation, and the subcortical seed regions were selected from 36 subregions in the human Brainnetome atlas 7, which were dimensionality reduced into 7 preserved network structures 8. We employed the network-based statistic approach to identifying the functional connectome patterns of the individual difference in distress during COVID-19 pandemic. To evaluate the predictive performance of brain connectome, we conducted prediction analyses using 10-fold cross-validation with linear regression. Consequently, we performed the mediation analysis to investigate the role of CPTSS in the association between functional connectome and distress symptoms during COVID-19.
Results
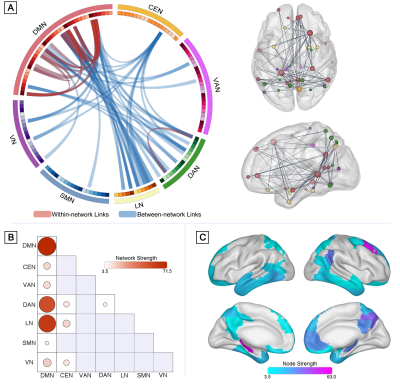
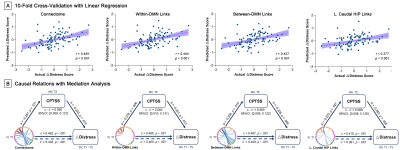
The distress symptoms evaluated by DASS did not differ significantly in pre- and during-pandemic period (t99 = 1.36, p = .176). In addition, significant associations of difference in distress with CPTSS were detected (r = -0.35, p = .001) when regressing out age, sex, head motion, socio-economic status, and the score of self-rating life events checklist.The general linear model identified distress-related brain functional connectome with 70 connections after NBS-based correction. The individual connection strength of connectome allowed prediction of the alteration in distress during COVID-19 after controlling for age, sex and head motion (r ranged from 0.33 to 0.39, all p ≤ .001), and smaller connected pair strength predicted severer distress symptoms after pandemic outbreak. Among these identified links, 20 links were assigned to within-network pairs and 50 links to between-network pairs. Notably, most of the within-network connections located in the DMN (19/20 links, network strength = 77.44), and links between the DMN and LN (17/50 links, network strength = 63.45) and links between the DMN and DAN (15/50 links, network strength = 55.78) constituted the largest proportion of between-network pairs. The node strength analysis revealed that the left caudal hippocampus (node strength = 63.08, belonging to DMN), right dorsomedial prefrontal cortex (node strength = 56.26, belonging to DMN), and right precuneus (node strength = 37.76, belonging to CEN) are the top 3 provincial hubs with more than 10 connections, which may play a critical role in connectome resilience and robustness. Analysis of 10-fold cross-validation with linear regression suggested that the prediction of distress via functional connectome was found to be reliable (r = 0.46, p < .001).The difference in distress could also be predicted by the within-DMN links (r = 0.44, p < .001), between-DMN links (r = 0.43, p < .001), and left caudal hippocampal links (r = 0.38, p < .001), respectively.
The mediation analyses demonstrated that the CPTSS partially explained the connectome-distress linkage (standard indirect effect = 0.06; 95% CI = [0.01, 0.12]) when controlling for age, sex, and head motion. The mediation model held true when selecting within-DMN, between-DMN, and left caudal hippocampal links as independent variables.
Conclusions
In the prospective investigation of public mental health following the unprecedented COVID-19 pandemic, we assessed the psychological status of a general sample in the pre-pandemic, outbreak and remission periods. The general levels of distress did not differ between pre- and during-pandemic phases, but the alterations of distress were associated with pandemic-related posttraumatic stress symptoms. Furthermore, we built a brain-distress construct which mainly contained within- and between-DMN connection patterns, and the left caudal hippocampus emerged as the hub region in distress-related connectome. Based on the predisposing customized brain connectome, we may identify individuals who confer high vulnerability to pandemic-induced long-standing distress symptoms with well-performing predictive modeling. In this case, our findings may facilitate the understanding of neural correlates underlying pandemic-induced distress on the individual macro-scale network level, and the susceptibility markers may serve as targets for early prevention and psychological intervention.Acknowledgements
Funding Statement This work was supported by the National Natural Science Foundation of China (Q.Y.G., grants 81621003 and 82027808), (S.W., grant 31800963); the National Natural Science Foundation (J.S. and Q.Y.G., grant 81820108018).References
1 Zavlis O, Butter S, Bennett K, Hartman TK, Hyland P, Mason L, et al. How Does the COVID-19 Pandemic Impact on Population Mental Health? A Network Analysis of COVID Influences on Depression, Anxiety and Traumatic Stress in the UK Population. Psychol Med 2021. doi:10.1017/S0033291721000635.
2 Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020; 87: 40–8.
3 Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional Distress in Young Adults during the COVID-19 Pandemic: Evidence of Risk and Resilience from a Longitudinal Cohort Study. Psychol Med 2020. doi:10.1017/S003329172000241X.
4 Prout TA, Zilcha-Mano S, Aafjes-van Doorn K, Békés V, Christman-Cohen I, Whistler K, et al. Identifying Predictors of Psychological Distress During COVID-19: A Machine Learning Approach. Front Psychol 2020; 11: 1–14.
5 Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun 2020; 87: 49–50.
6 Chin Fatt CR, Jha MK, Cooper CM, Fonzo G, South C, Grannemann B, et al. Effect of Intrinsic Patterns of Functional Brain Connectivity in Moderating Antidepressant Treatment Response in Major Depression. Am J Psychiatry 2020; 177: 143–54.
7 Fan L, Li H, Zhuo J, Zhang Y, Wang J, Chen L, et al. The Human Brainnetome Atlas: A New Brain Atlas Based on Connectional Architecture. Cereb Cortex 2016; 26: 3508–26.
8 Schaefer A, Kong R, Gordon EM, Laumann TO, Zuo X-N, Holmes AJ, et al. Local-Global Parcellation of the Human Cerebral Cortex from Intrinsic Functional Connectivity MRI. Cereb Cortex 2018; 28: 3095–114.
Figures