3749
Cerebrovascular dysfunction leads to related Gray Matter loss in HIV infection
Bei Wang1, He Wang1,2, Ying-Hua Chu3, Yuxin Shi4, Dan-Chao Cai4, and Yi Zhan4
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Human Phenome Institute, Fudan University, Shanghai, China, 3MR Collaboration, Siemens Healthineers Ltd., Shanghai, China, 4Radiology department,Shanghai Public Health Clinical Center, Fudan University, Shanghai, China
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Human Phenome Institute, Fudan University, Shanghai, China, 3MR Collaboration, Siemens Healthineers Ltd., Shanghai, China, 4Radiology department,Shanghai Public Health Clinical Center, Fudan University, Shanghai, China
Synopsis
We examined the effects of HIV on the structure of cerebrovasculature and the interactions among HIV infection, brain tissue volume and cerebrovascular structure. Decreased cerebral vessel volume, vessel length and branch number were found in people with HIV. HIV related gray matter loss was found caused by the decreasing vessel length. Additionally, decreasing vessel distribution in left insula was found in vessel probability atlas in people with HIV, which may relate to various clinical symptoms.
Introduction
Human immunodeficiency virus (HIV) enters the brain at the very beginning of infection. Studies from the past 20 years about HIV effects on brain reported lower GMV and lower WMV consistently [1,7]. A recent work has proved HIV infection a cause of blood-brain barrier (BBB) disruption [2], which affects the blood supply to relevant brain areas directly. Furthermore, clinical studies show that HIV-associated vasculopathies prefer medium and large vessels[3,5,6]. Thus, we hypothesize that the structure of cerebrovascularture changes with HIV infection.Methods
A cross-sectional study with prospective enrollment of 102 people with HIV (PWH) and frequency age- and sex-matched 51 HIV-uninfected controls (HUC) was carried out from HIV department and Health Examination Center of Shanghai Public Health Clinical Center, between 2019 and 2021. All participants signed informed consent prior to the research.The MRI data including T1 and TOF images were acquired on 3T MAGNETOM Skyra (Siemens Healthcare, Erlangen, Germany). The scanning protocol included whole-brain 2D T1 dark-fluid sequence (repetition time [TR]/effective echo time [TE] 2000/9ms; voxel size 0.69x0.69x6.8mm) and multi-slab TOF sequence (repetition time [TR]/effective echo time [TE] 21/3.69ms; voxel size 0.4x0.4x0.8mm).
All MRI scans were reviewed for quality before analysis. Subjects with motion artifacts were excluded.
To examine the cerebrovascular features, we developed a workflow to quantitative estimate cerebrovascular features automatically based on TOF images. Independent-samples T test was used to assess the impact of HIV on brain structure, including grey matter volume (GMV), white matter volume (WMV) and cerebrovascular morphologies. Volume based Morphometry analysis (VBM) was applied to T1 magnetic resonance imaging (MRI) data to estimate structural changes of brain tissue. Cerebrovascular probability atlases were generated in each group. The probability atlas was overlaid on VBM results in MNI space to determine the spatial relationship between cerebral vessels and the affected brain tissue.
In order to investigate the interactions among HIV, cerebrovascular morphologies and brain tissue volume, mediator analysis was completed.
Results and Discussion
94 PWHs and 50 HUCs were included in the final analyses. For the PWH and the HUG group, the mean (SD) age was 35.03 and 38 years respectively, among whom 94% and 88%, respectively, were men. In the PWH group, 78 participants were treated, and treatment information of 4 participants were not documented.HIV infection effects on Cerebrovascular Structure and Brain tissue Volume, respectively.
For the cerebrovascular features, lower cerebral vessel volume (p = 0.001), vessel density (p = 0.01), shorter length (p = 0.001) and less branches (p = 0.021) were observed in the PWH group. Additionally, no significant difference in averaged cerebral vessel radius and tortuosity were evident between groups. As to brain tissue, significant decrease in GMV and WMV were identified, in accordance with results from previous reports, in the PWH group(Table 1). Cerebral vessel atlases in MNI space were generated using 46 PWH and age- and sex-matched 46 HUCs (Figure 1).
Altered brain area obtained by VBM analysis was overlaid with the cerebrovascular probability atlases in the MNI space. Altered brain areas were found adjacent to the locations of cerebral vessels mostly (Figure 2).
Brain tissue Volume Associate with Cerebrovascular Structure
Vessel length, tortuosity and vessel volume were all associated with both GMV and WMV (p<0.05). Correlations between these cerebrovascular features and GMV still exist after adjusting for risk factors including age, sex, HIV infection and treatment. Moreover, positive association between vascular radius and GMV was found (p = 0.035)(Table 2).
Based on the results from previous analyses, cerebrovascular length and volume were distinguished relating to both brain structure and HIV infection. As a result, HIV infection was considered an indirect pathway acting on brain volume by affecting cerebral vessels.
Interaction among HIV infection, Cerebrovascular Structure and Brain tissue Volume
To test the interaction, mediator analysis was completed with cerebrovascular features as mediators.The models were simplified by using cerebrovascular length as the only mediator, as vessel volume is highly related to vessel length and radius. Cerebrovascular radius and tortuosity were considered covariances as they were associated with GMV.
With the addition of mediator, direct effect of HIV infection on GMV disappeared (p > 0.05)(Figure 3). HIV infection was found to indirectly impact GMV by affecting cerebrovascular length (effect = -0.0066, BootLLCI = -0.017, BootULCI = -0.0006), which suggest complete mediating effect. The whole model was reliable (R2 = 0.354, p < 0.001) and indicated that HIV infection affects brain structure mostly by reducing cerebral vessels length.
Conclusion
After adjusting for age and sex, HIV infection is associated with decrease in cerrebrovascular structure. Decreased vessel length can be caused by vascular dysfunction, including reduction of blood flow or damage in vessel wall. Therefore, complete mediating effect suggests HIV related gray matter loss is mainly caused by cerebrovascular dysfunction. Decreased vessel distribution in left insula area suggests multifaceted effects on brain function.Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81971583), National Key R&D Program of China (No. 2018YFC1312900), Shanghai Natural Science Foundation (No. 20ZR1406400), Shanghai Municipal Science and Technology Major Project (No.2017SHZDZX01, No.2018SHZDZX01) and ZJLab.References
- O'Connor EE, Zeffiro TA, Zeffiro TA. Brain Structural Changes following HIV Infection: Meta-Analysis. AJNR Am J Neuroradiol. 2018 Jan;39(1):54-62. doi: 10.3174/ajnr.A5432. Epub 2017 Nov 2. PMID: 29097412; PMCID: PMC7410705.
- Bertrand L, Cho HJ, Toborek M. Blood-brain barrier pericytes as a target for HIV-1 infection. Brain. 2019 Mar 1;142(3):502-511. doi: 10.1093/brain/awy339. PMID: 30668645; PMCID: PMC6391611.
- Edwards NJ, Grill MF, Choi HA, Ko NU. Frequency and Risk Factors for Cerebral Arterial Disease in a HIV/AIDS Neuroimaging Cohort. Cerebrovasc Dis. 2016;41(3-4):170-6. doi: 10.1159/000442755. Epub 2016 Jan 12. PMID: 26751784; PMCID: PMC4788563.
- Jerman T, Pernus F, Likar B, Spiclin Z. Enhancement of vascular structures in 3d and 2d angiographic images. Ieee Transactions on Medical Imaging. 2016;35:2107-2118
- Monsuez J J, Charniot J C, Escaut L, et al. HIV-associated vascular diseases: structural and functional changes, clinical implications[J]. International journal of cardiology, 2009, 133(3): 293-306.
- Shenoy A, Dwork A, Elkind MSV, Marshall R, Morgello S, Gutierrez J. Brain Large Artery Lymphocytic Inflammation and Human Immunodeficiency Virus-Related Brain Arterial Remodeling. J Virol. 2018 May 29;92(12):e00081-18. doi: 10.1128/JVI.00081-18. PMID: 29618649; PMCID: PMC5974492.
- Leite SC, Corrêa DG, Doring TM, Kubo TT, Netto TM, Ferracini R, Ventura N, Bahia PR, Gasparetto EL. Diffusion tensor MRI evaluation of the corona radiata, cingulate gyri, and corpus callosum in HIV patients. J Magn Reson Imaging. 2013 Dec;38(6):1488-93. doi: 10.1002/jmri.24129. Epub 2013 Apr 4. PMID: 23559497.
Figures
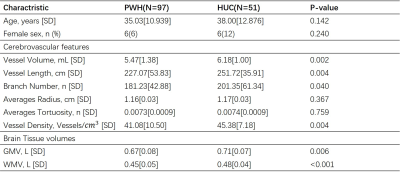
Table 1.Independent T test for comparasion of demographics, cerebrovascular morphologies and brain tissue volume between PWH and HUC groups.
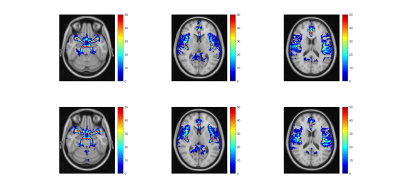
Figure 1.Comparasion of cerebrovascualr possibility atlases between PWH (the upper colume) and HUC (the lower colume) groups.
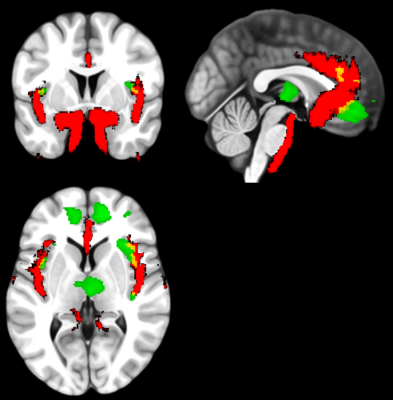
Figure 2.The overlap (in yellow) areas in MNI space of vessel distribution area (in red) and the altered gray matter regions (in green).
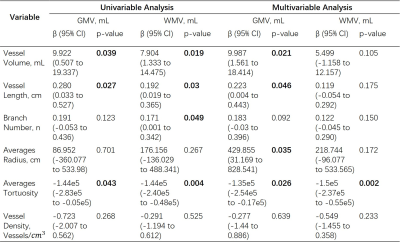
Table 2.Association between erebrovascular features and brain tissue volumes in univariable analysis and multivariable analysis adjusting for age, sex, HIV infection and treatment or not.
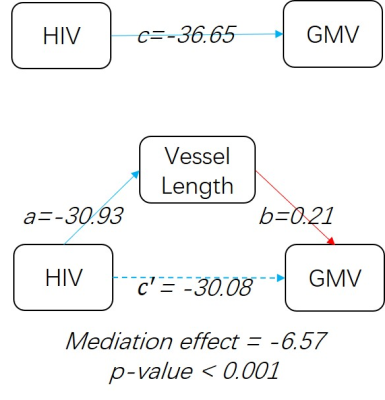
Figure 3.Mediation analysis results considering vessel length as mediator and averaged vascualr radius and tortuosity as covariances. Red line represents a positive relation, and blue lines represent negatively.
DOI: https://doi.org/10.58530/2022/3749