3747
Can combined 3D pcASL and t-ASL imaging effectively assess collateral compensation for patient with unilateral MCA severe stenosis or occlusion?
juan li1, guangrui shao1, and weiqiang dou2
1The Second Hospital of Shandong University, jinan, China, 2MR Research, GE Healthcare, beijing, China
1The Second Hospital of Shandong University, jinan, China, 2MR Research, GE Healthcare, beijing, China
Synopsis
This study aimed to compare the difference of blood perfusion and collateral circulation compensation between symptomatic and asymptomatic patients with severe stenosis or occlusion of unilateral middle cerebral artery (MCA) by using 3D pseudo-continuous arterial spin labeling (pcASL) at two different post labeling delays (PLD) times of 1.5s and 2.5s and territorial pcASL with bilateral internal carotid arteries, ipsilateral external carotid artery and vertebrobasilar artery labelled. 49 patients (26 symptomatic and 23 asymptomatic) were recruited. Compared with symptomatic group, asymptomatic group showed significantly stronger collateral circulation and higher number of patients with secondary collateral circulation opening.
Introduction
Intracranial arterial occlusion can lead to ischemic necrosis of brain tissue in local blood supply area, and the existence of collateral circulation plays an important role in maintaining cerebral perfusion and metabolism [1]. Patients with good collateral circulation can avoid the occurrence of cerebral infarction and thus have a good prognosis [2]. At present, digital subtraction angiography is the reference in evaluating collateral circulation. The invasive property however limits its clinical applications [3].3D pseudo-continuous arterial-spin-labeling (3D-pcASL) is a well established non-invasive perfusion imaging to quantitatively measure cerebral blood flow (CBF). Different post-label-delay (PLD)s applied in 3D-pcASL allow for evaluating CBF at different flow velocity comprehensively [4]. 3D territorial-ASL (t-ASL) was a further developed ASL technique based on 3D-pcASL, allowing for CBF measurement of specific vessel labeled. With these advantages of both techniques, the formation and the source of collateral circulation on the side of vascular occlusion may be observed [5]. Therefore, this study aimed to evaluate the formation of collateral circulation between symptomatic and asymptomatic patients after severe stenosis or occlusion of unilateral middle cerebral artery (MCA) by using 3D-pcASL at two different PLDs and t-ASL. The prognosis of patients was also assessed.Materials and methods
Subjects 49 patients (28 male vs 21 female, age: 63.27±12.02 years) with severe stenosis or occlusion of unilateral MCA, defined as the stenotic degree ≥ 75% by MRA, were included in this study. These patients were classified into symptomatic group (n=26) and asymptomatic group (n=23) according to whether notable symptoms occurred in the blood supply area of diseased vessels for half a month. Symptomatic group included patients with cerebral infarction and patients with transient ischemic attack (TIA).MRI experiment 3D-pcASL and t-ASL measurements were performed on a 3T-MRI scanner (GE signa pioneer, USA) with 29-channel head & neck coil for each patient. For 3D-pcASL,PLDs of 1.5 and 2.5ms were applied. For t-ASL, bilateral internal carotid arteries, ipsilateral external carotid artery and vertebrobasilar artery were separately labelled. Other scan parameters were listed in Table 1. Total scan time was about 30 mins.
Image analysis 3D-pcASL and t-ASL data were post-processed in vendor-provided software on GE Advanced Workstation 4.6. 3D-pcASL derived CBF and vessel-specific CBF mapping from t-ASL were obtained for each patient accordingly.On CBF maps of 3D-pcASL, regions of interest (ROI)s with size of 15-20cm2 were manually drawn on the blood supply region of MCA close to lateral ventricle. PLD specific CBF levels of both affected and contralateral MCA were obtained for each patient. Vessel-specific CBF maps from t-ASL were used to assess the formation of collateral compensation in the blood supply area of affected MCA between two patient groups. Together with MRA, t-ASL was also used to analyze the opening of secondary collateral circulation.
Statistical Analysis All statistical analyses were performed in SPSS 22.0. Independent sample T-test or Mann-Whitney U-test was used for measurement data, and Chi-square test was applied for count data. PLD specific CBF values of MCA supply area at two patient groups were used for inter-group comparison with independent sample T-test, and intra-group comparison with paired sample T-test. Receiver-operating-characteristic (ROC) curve analysis and area-under-the-curve (AUC) were used to evaluate the separate diagnostic efficacy of CBF at PLD1.5s and PLD2.5s in distinguishing symptomatic from asymptomatic patients. Chi-square test or Fisher's test was used to compare the collateral compensation of the blood supply area of affected MCA on vessel-specific CBF maps between two patient groups. The sources of collateral compensations were counted. P<0.05 was considered statistical significance.
Results
Comparable clinical factors, including age, gender, hypertension, diabetes mellitus, smoking and drinking, were found between two patient groups (Table.2). Compared with asymptomatic group, symptomatic group showed significantly lower CBF in both affected and contralateral side of MCA at both PLDs (all P<0.05;Table.3).CBFs at both PLDs were significantly different between the affected and contralateral side for symptomatic group (P<0.05). Meanwhile, this difference was only revealed at PLD1.5s for asymptomatic group (P <0.05). Additionally, on the affected side, the CBF increase of MCA from PLD1.5s to 2.5s was statistically higher in asymptomatic than symptomatic group (P<0.001). Using ROC analysis, CBF at PLD2.5s showed higher clinical efficacy than at PLD1.5s in distinguishing symptomatic from asymptomatic patients (Figure.1).On vessel-specific CBF maps, compared with asymptomatic group, symptomatic group showed significantly less collateral compensation in the affected MCA (P<0.05; Figs2,3). Meanwhile, significantly higher patients with secondary collateral compensation were found in asymptomatic than symptomatic group (P<0.05). Moreover, for patients with collateral compensation, the compensations were mostly found from vertebrae-basilar artery, and the rest were from the contralateral internal carotid artery or ipsilateral external carotid artery.Discussion and Conclusion
In this study, relative to symptomatic patients, asymptomatic patients revealed stronger collateral perfusion, and larger number of patients with secondary collateral compensatory opening. This might explain why asymptomatic patients had no symptoms, and symptomatic patients showed different outcomes depending on the amount of collateral compensation. In conclusion, combined multi-PLD 3D-pcASL and t-ASL might provide a comprehensive assessment of collateral compensation for patients with unilateral middle cerebral artery severe stenosis or occlusion.Acknowledgements
NONEReferences
[1] Wei W, Yi XY, Ruan JH, et al. Influence of collateral circulation on cerebral blood flow and frontal lobe cognitive function in patients with severe internal carotid artery stenosis[J]. BMC Neurol, 2019, 19(1):151.[2] Hartkamp NS, Petersen ET, Chappell MA, et al. Relationship between haemodynamic impairment and collateral blood flow in carotid artery disease[J]. J Cereb Blood Flow Metab, 2018, 38(11):2021-2032. [3] Verdolotti T, Pilato F, Cottonaro S, et al. ColorViz, a New and Rapid Tool for Assessing Collateral Circulation during Stroke[J]. Brain Sci, 2020, 10(11):882. [4] Choi HJ, Sohn CH, You SH, et al. Can Arterial Spin-Labeling with Multiple Postlabeling Delays Predict Cerebrovascular Reserve ?[J]. AJNR Am J Neuroradiol, 2018, 39(1):84-90. [5] Hartkamp NS, Petersen ET, De Vis JB, Bokkers RP, Hendrikse J. Mapping of cerebral perfusion territories using territorial arterial spin labeling: techniques and clinical application[J]. NMR Biomed, 2013, 26(8):901-12.Figures
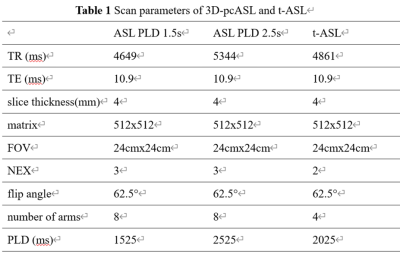
Table 1 Scan parameters of 3D-pcASL and t-ASL
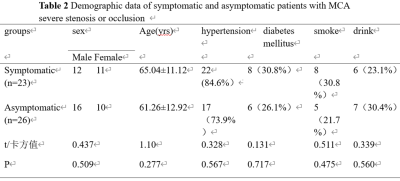
Table 2 Demographic data of symptomatic and asymptomatic patients with MCA severe stenosis or occlusion
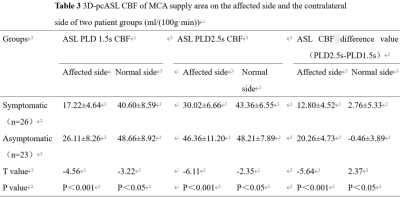
Table 3 3D-pcASL CBF of MCA supply area on the affected side and the contralateral side of two patient groups (ml/(100g·min))
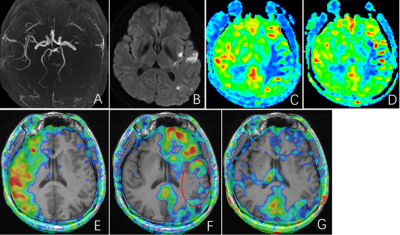
Figure 2 a 32-years-old, male, symptomatic patient. (A) left MCA occlusion showing in MRA. (B) High DWI signal in left temporal lobe. (C) Significantly reduced perfusion in the left MCA blood supply area at PLD1.5s. (D) Better perfusion in the left MCA blood supply area at PLD2.5s, although it was still lower than the contralateral side. (E-G) t-ASL imaging shows the right ICA, the left ICA and the vertebrobasilar artery, respectively. The left MCA blood supply area was hypoperfusion (red circle), and no compensation from contralateral ICA or vertebrobasilar artery was observed.
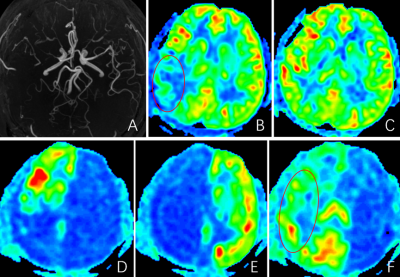
Figure 3 a 29-years-old, male, asymptomatic patient. (A) Subtotal occlusion of the MCA on the right side showing in MRA. (B) Decreased perfusion in the right MCA blood supply area at PLD1.5s (red circle). (C) Comparable perfusion of left and right cerebral hemispheres at PLD2.5s. (D-F) t-ASL imaging shows the blood supply area of right ICA, left ICA and vertebrobasilar artery respectively, and the right ICA has insufficient perfusion. The hypoperfusion area of the right MCA is completely compensated by the vertebrobasilar artery of the posterior circulation (red circle).
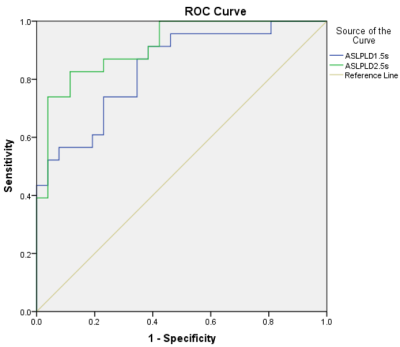
Figure 1 The ROC curve shows the sensitivity and specificity values for distinguishing symptomatic from asymptomatic patients of ASL PLD 1.5s and ASL PLD 2.5s at various levels of cut-off scores. ASL PLD 2.5s (AUC=0.913;95%CI:0.835-0.991 P<0.05) is higher than ASL PLD 1.5s (AUC=0.838;95%CI:0.727-0.948 P<0.05).
DOI: https://doi.org/10.58530/2022/3747