3739
The combination of DCE-MRI and IVIM to differentiate rectal mucinous adenocarcinoma and tubular adenocarcinoma1The First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Dalian Medical University, Dalian, China
Synopsis
The purpose of this study is to use IVIM(intravoxel incoherent motion)and DCE(dynamic contrast-enhanced)imaging techniques to identify the value of rectal mucinous adenocarcinoma and tubular adenocarcinoma, and to provide rich information and help for clinical decision-making.
Abstract
SynopsisThe purpose of this study is to use IVIM(intravoxel incoherent motion)and DCE(dynamic contrast-enhanced)imaging techniques to identify the value of rectal mucinous adenocarcinoma and tubular adenocarcinoma, and to provide rich information and help for clinical decision-making. The results show that the quantitative values of stand ADC, D and kep of rectal mucinous adenocarcinoma are significantly different from those of rectal ductal adenocarcinoma, and the combined effect is higher.In this study, we aim to use IVIM imaging combined with DCE imaging to explore the value of rectal mucinous adenocarcinoma and tubular adenocarcinoma. Combining IVIM and DCE values can obtain higher diagnostic efficacy (AUC: 0.800; sensitivity: 79%; specificity: 80%).Introduction As the third most common and fatal malignant tumors in the world, rectal tubular adenocarcinoma has been closely concerned[1]. Because of the similar signals, it is difficult for traditional MR imaging methods to distinguish rectal mucinous adenocarcinoma from tubular adenocarcinoma. Mucinous adenocarcinoma has a higher degree of malignancy. Studies have shown that mucinous adenocarcinoma is an independent risk factor for 3 lymph node metastases in patients with rectal cancer [2]. Accurate judgment before surgery is an urgent need for accurate diagnosis of rectal cancer.
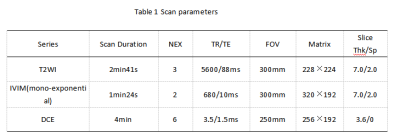
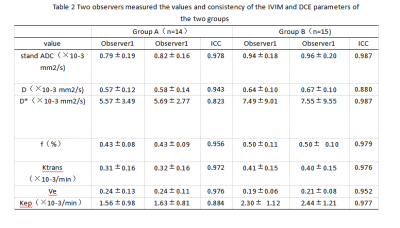
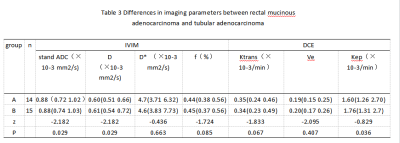
Materials and MethodsThis study has been approved by the local IRB. 29 patients with rectal cancer lesions were retrospectively analyzed, all patients were divided into two groups: 14 patients with rectal mucinous adenocarcinoma (group A, 10 males, 4 females, age 63.36±9.20 years) and 15 patients with tubular adenocarcinoma (group B, 11males, 4 female, age 67.00±2.81 years).All patients underwent abdominal MR examinations (Signa HDxt, GE Medical Systems, USA) included T2WI, IVIM and DCE(Scan parameters show in table 1). The original axial digital images from the IVIM sequence and DCE sequencewere transmitted to the GE SDC-ADW 4.6 workstation (Sun Microsystems, Santa Clara, Calif) and the post-processing was performed by Functool software. Referring to the anatomical location of lesion obtained on T2-weighted or DWI images, the stand ADC, D, D* , f and Ktrans,Ve, Kep maps were automatically constructed, and were reviewed by two observers who were blinded to clinical information and histopathologic results with 8 and 2 years of experience in rectal imaging, respectively. Three circle ROIs were manually placed on the slice with largest area of lesion with high signal intensity and obvious enhancement on IVIM and DCE images, respectively.(Fig. 1,2). The measurement was repeated for three times, and the averages of three measurements were calculated. The stand ADC, D, D* ,f and Ktrans,Ve, Kep were recorded. Intra-group correlation coefficient (ICC) was used to test the measurement consistency between the two observers. Difference between above values was compared by Mann-Whitney U test. Receiver operating characteristic (ROC) analysis was performed to evaluate diagnostic performance.
Result IVIM values and DCE values measured by the two observers were well consistent (ICC > 0.75)(table 2)stand ADC , D and Kep values showed significant difference between two groups (p<0.05)(table 3). Areas under the ROC curve (AUC) of stand ADC , D and Kep values were 0.793,0.729 and 0.733. The sensitivity and specificity of stand ADC , D and Kep values were 78.6%, 71.4%, and 63.6%,71.4%(Fig. 3). With combination of stand ADC,D and Kep values for rectal mucinous adenocarcinoma and tubular adenocarcinoma, the diagnostic efficacy become significantly increased (AUC=0.800), as well as the sensitivity (78.6%) and the specificity (80.0%) (Fig. 4).
Discussion and conclusionIVIM imaging combined with DCE imaging can effectively distinguish rectal mucinous adenocarcinoma and tubular adenocarcinoma[3,4]. The T1 value of the tubular adenocarcinoma group was significantly higher than that of the mucinous adenocarcinoma group.
Acknowledgements
NoneReferences
[1]Li Ming,Xu Xiaodan,Xia Kaijian et al. Comparison of Diagnostic Performance between Perfusion-Related Intravoxel Incoherent Motion DWI and Dynamic Contrast-Enhanced MRI in Rectal Cancer.[J] .Comput Math Methods Med, 2021, 2021: 5095940.
[2]Minutoli Fabio,Pergolizzi Stefano,Blandino Alfredo et al. Effect of granulocyte colony-stimulating factor on bone marrow: evaluation by intravoxel incoherent motion and dynamic contrast-enhanced magnetic resonance imaging.[J] .Radiol Med, 2020, 125: 280-287.
[3] Long L, Zhang H, He X, Zhou J, Guo D, Liu X. Quantitative evaluation of intravoxel incoherent motion diffusion-weighted imaging (IVIM) for differential diagnosis and grading prediction of benign and malignant breast lesions. Medicine (Baltimore). 2018 Jun;97(26):e11109.
[4]Kim HJJon, science. Variability in Quantitative DCE-MRI: Sources and Solutions.J Nat Sci. 2018;4(1):e484.
Figures
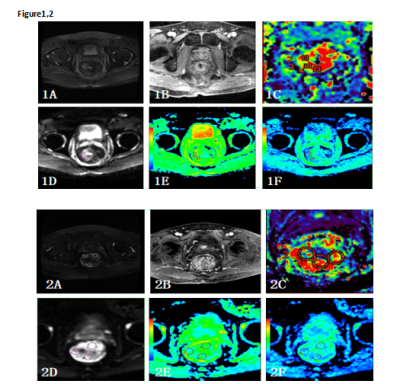
Figure 1 A 67-year-old male patient with the rectal mucinous adenocarcinoma. T2 image (1A), DCE original image (1B), and Kep image (1C) ,IVIM original image(1D), stand ADC image (1E), and D image (1F) were showed.
Figure 2 A 70-year-old male patient with the rectal tubular adenocarcinoma. T2 image (2A), DCE original image (2B), and Kep image (2C) ,IVIM original image(2D), stand ADC image (2E), and D image (2F) were showed.
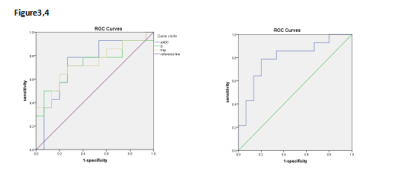
Figure3Areas under the ROC curve (AUC) of stand ADC , D and Kep values were 0.793,0.729 and 0.733. The sensitivity and specificity of stand ADC , D and Kep values were 78.6%, 71.4%, and 63.6%,71.4%.
Figure4With combination of stand ADC,D and Kep values for rectal mucinous adenocarcinoma and tubular adenocarcinoma, the diagnostic efficacy become significantly increased (AUC=0.800), as well as the sensitivity (78.6%) and the specificity (80.0%) .