3733
Combining diffusion kurtosis imaging and clinical data for predicting the extramural venous invasion of rectal adenocarcinoma1The Second Clinical College of Guangzhou University of Chinese Medicine, Guangzhou, China, 2the Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, China, 3Philips Healthcare, Guangzhou, China
Synopsis
The extramural venous invasion (EMVI) is considered as the potential prognostic factor for patients with rectal carcinoma. We tried to investigate the diagnostic ability of diffusion kurtosis imaging (DKI) - derived parameters as risk factors for EMVI’s involvement status.Our results showed that the Kmean values, lymph node involvement, and an advanced tumor stage (T3) were independent risk factors for the prediction of EMVI status, which may suggest that the DKI as a potential biomarker for evaluating the EMVI status of rectal cancer is feasible.
Background
The presence of EMVI has been recognized as an essential and independent, yet unfavorable and prognostic factor for patients with rectal carcinoma, particularly due to its association with local nodal involvement, the development of distant metastases, recurrence, and impaired survival outcomes [1-5]. Therefore , it is important to identify the EMVI status of rectal carcinoma. Here, we investigated the diagnostic ability of diffusion kurtosis imaging (DKI) -derived parameters as risk factors for EMVI’s involvement status in rectal adenocarcinoma.Methods
This retrospective study recruited 154 consecutive patients with locally advanced rectal cancer who underwent a 3.0 Tesla MR examination (Ingenia, Philips Healthcare, Best, The Netherlands) before surgery. DKI was scanned with b values of b=0 s/mm2, 600s/mm2 , 1000 s/mm2, and 2000 s/mm2 . The Kmean, Dmean, and apparent diffusion coefficient (ADC) values were calculated. Moreover, the clinical information, serum tumor markers, MR manifestations, and pathological changes of EMVI were assessed. With the postoperative pathological result as the gold standard, the patients were divided into the EMVI-positive group (n=63) and EMVI-negative group (n=91). Spearman's rank correlation coefficient was used to explore the relationship between those parameters and mrEMVI scores. Differences between the two groups were compared using the t-test or Mann-Whitney U test depends on the results of normality test. Univariate and multivariate logistic regression analyses were performed to identify factors significantly associated with pEMVI, and odds ratios (OR) sidelong with 95% CI were calculated. Receiver-operating characteristic curve analysis was performed to evaluate the diagnostic performance. Statistical significance was defined as p < 0.05.Results
Among the 154 patients, pEMVI-positive rectal tumors had significantly higher Kmean values and lower ADCmean values compared to those in pEMVI-negative rectal tumors. Kmean values positively correlated with mrEMVI scores (r = 0.343, p < 0.001), whereas ADCmean values showed negative correlation with mrEMVI scores (r = -0.262, p = 0.001). However, there was no significant correlation between the Dmean values and the mrEMVI scores (r = 0.025, p = 0.760). Univariate analysis demonstrated that the increased Kmean values, decreased ADCmean values, nodal involvement, an advanced tumor stage, and a G2 tumor grade were significantly related to the pEMVI of rectal adenocarcinoma (Table 1). The multivariate analysis demonstrated that the Kmean values, lymph node involvement and an advanced tumor stage (T3) were independent risk factors for the prediction of EMVI status. This model showed excellent diagnostic performance for prediction of EMVI status. (AUC = 0.835, P < 0.001,Figure 3 )Conclusions
The potential of DKI as a biomarker for evaluating the EMVI status of rectal cancer is feasible, especially given DKI’s capability of detecting tumor heterogeneity noninvasively.Acknowledgements
No acknowledgement found.Figures
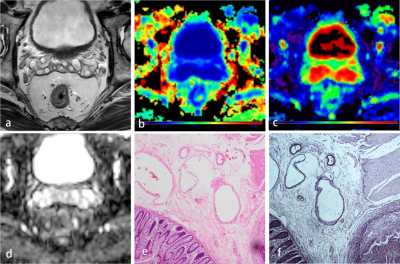
Figure 1 : image in a 46-year-old male with grade 2 rectal adenocarcinoma with negative pEMVI. (a) Axial T2-weighted MRI shows slightly low–signal-intensity rectal mass (b) Kurtosis map demonstrates the lesion with a Kmean value of 0.95. (c) Diffusion map shows the lesion with a Dmean value of 1.28×10-3 mm2/sec. (d) The apparent diffusion coefficient map shows a low-intensity tumor (ADC mean value 1.16×10-3 mm2/sec). (e, f) Histological (hematoxylin and eosin and corresponding elastin trichrome staining) analyses demonstrated no evident venous invasion (×40).
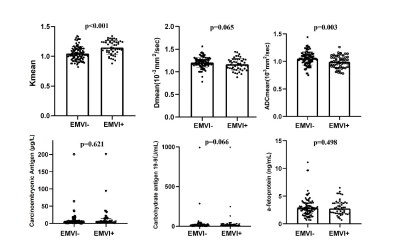
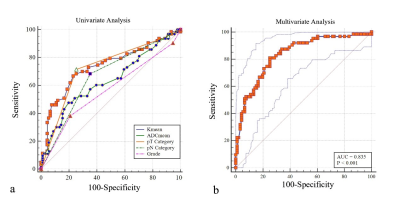
Figure 3 : Receiver operating characteristic curves of univariate analysis and multivariate analysis for predicting positive EMVI status of rectal adenocarcinoma. Details of the area under the curves for each index are shown in the results section.