3718
Machine learning and the prediction of cerebral ventricular changes in fetuses with ventriculomegaly: a fetal MRI study
1Department of Radiology, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Suzhou city, Jiangsu province, 215002, China, 2Department of Radiology, The First Affiliated Hospital of Soochow University, Suzhou city, Jiangsu province, 215000, China, 3Institute of Medical Imaging, Soochow University, Suzhou city, Jiangsu province, 215000, China, 4National Clinical Research Center for Hematologic Diseases, the First Affiliated Hospital of Soochow University, Suzhou city, Jiangsu province, 215000, China
Synopsis
Fetal ventriculomegaly (FV) is one of the central nervous system (CNS) major malformations. Prenatal clinical research has seen only a few applications of machine learning. To our knowledge, radiomic machine learning for predicting the change of cerebral ventricular in fetuses with ventriculomegaly has not been reported. We discovered that a combination of clinical characteristics and fetal MRI features could accurately predict postnatal ventricular changes in fetuses with ventriculomegaly. The occipital lobe white matter on the dilated lateral ventricle side may play an important role in the pathophysiological process in FV.
Introduction
FV is determined by ventricular measurements taken at the level of the ventricular atrium and a minimum cutoff of 10 mm1-2. FV stabilizes in about 55 percent of patients and resolves in 30 percent3. The occipital horns of the lateral ventricle are the first to dilate in embryonic ventriculomegaly4. It's still unclear whether occipital white matter neuroimaging radiomics can predict postnatal ventricular changes in FV. Machine learning has been used to predict which fetuses with ventriculomegaly needed a cerebrospinal fluid shunt after delivery5 and in fetal brain age estimation and fetal anomaly detection based on fetal MRI features6. It's critical to use machine learning to figure out which characteristics can be used to predict the ventricle changes in FV, which can not only provide personalized guidance to prospective parents while reducing unnecessary imaging examinations. Our goal is to find out whether using machine learning approaches to extract various parameters from clinical characteristics and fetal MRI imaging can predict the changes in cerebral ventricular in fetuses with ventriculomegaly after delivery.Methods
Subjects: We used retrospective case-control research from January 1, 2013, to June 30, 2021. All fetuses with ventriculomegaly were initially detected using ultrasonography, then advised to have fetal MRI to rule out other additional intracranial disorders. A total of 95 fetuses with ventriculomegaly (27 female, gestational age range: 23.57~36.29 weeks) were scanned on an MRI system (Philips Achieva; Philips Medical Systems, Best, the Netherlands) with a 5-channel cardiac coil. The fetuses were separated into two groups, with one group consisting of 66 fetuses with ventriculomegaly resolved and the other consisting of 29 cases with ventriculomegaly stable after delivery. The institutional review board at the Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, accepted the research and waived the requirement for permission for this retrospective cohort study.Acquisition Protocol: T2-weighted single-shot fast-spin echo (SSFSE) was performed in the coronal, sagittal, and axial planes of fetal brain with the following parameters: TR/TE = 566ms/150ms; slice thickness = 3~4mm; intersection slice gap = -1~1mm; matrix = 200 x 135~256 x 256; FOV = 180~230mm; number of slices = 12 to 24.
Data Processing and Analysis: Clinical data included the maternal body mass index (BMI) and the fetus gestational age (GA). Measurements of the atrial diameter of the lateral ventricles (AD), the fronto-occipital horn ratio (FOHR) , the major and minor axis lengths of each occipital horn were calculated on the same axial section at the level of the atria of the lateral ventricles and the glomus of the choroid plexus5,7. The FOHR is the mean of the maximum frontal (a) and occipital horn diameters (b) divided by the biparietal diameter (BPD) [(a + b)/2BPD]5,7. All of the 2-dimensional (2D) area measurements were manually obtained using measurement tools in RadiAnt DICOM Viewer 4.0.3. ITK-SNAP (version 3.4.0) software was used to delineate the occipital lobe white matter on the dilated side8. To extract radiomics features, Pyradiomics (version 3.0.1) was utilized.T-test, logistic regression, and/or least absolute shrinkage and selection operator cross validation (Lasso CV) feature selection and feature downscaling were conducted. In a 7:3 ratio, all cases were assigned to training and test sets. Firstly, the occipital lobe white matter radiomics on the dilated side were modeled using the Gaussian NB method. After that, the clinical features, 2D measurements of the lateral ventricle, and white matter radiomics were combined to predict the changes of fetal lateral ventricles. The accuracy, sensitivity, specificity, and receiver operating characteristic (ROC) curves with the corresponding area under the curve (AUC) values were used to evaluate the training and test sets' classification performance.
Results
In the FV resolved group and FV stabilized group, there were 66 cases in the training set (46 cases resolved, 20 cases stabilized) and 29 cases in the test set (20 cases resolved and 9 cases stabilized). On the dilated side of the ventricle, 1619 radiomics features were retrieved from the occipital lobe white matter. Eight significant radiomics features were acquired after two rounds of t-test and Lasso CV feature screening (Figure 1). The accuracy, sensitivity, specificity, and AUC values of the training and test sets were 0.7273, 0.6739, 0.8500, 0.8652 and 0.7586, 0.7500, 0.7778, 0.7500, respectively (Figure 2A and 2B).After the model combination of white matter radiomics, pregnant maternal BMI, GA, and 2D diameters of the lateral ventricle (Figure 3), the accuracy, sensitivity, specificity, and AUC values of the training and test sets were 0.8444, 0.9375, 0.6154, 0.9423 and 0.7500, 0.8333, 0.5000, 0.8333, respectively (Figure 4A and 4B).
Discussion
Our findings reveal that radiomic characteristics derived from the occipital lobe white matter on the dilated side of the fetal ventricle can predict lateral ventricle alterations in fetuses with ventriculomegaly . The occipital lobe white matter on the dilated side may play an important role in the pathophysiological process in FV. The prenatal MRI features may be useful to predict the progression of cerebral ventricular in fetuses with ventriculomegaly based on machine learning approaches.Conclusion
For the first time, it is proposed that occipital white matter radiomics in FV might be employed as biological indicators for the changes of ventricular dilatation.Acknowledgements
This work was supported by the program for Gusu Medical Talent of Suzhou City [grant number GSWS2020009]; the Translational Research Grant of NCRCH [grant number 2020WSB06]; the National Natural Science Foundation of China [grant number 81671743]; the Clinical Key Diseases Diagnosis and Therapy Special Project of Health and Family Planning Commission of Suzhou [grant number LCZX201801]; the program for Advanced Talents within Six Industries of Jiangsu Province [grant number WSW-057]; and the High-level Health Personnel ‘six-one’ Project of Jiangsu Province in China [grant number LGY2016035].
References
1. Goynumer G, Yayla M, Arisoy R, et al. The criterion value of fetal cerebral lateral ventricular atrium width for diagnosis of ventriculomegaly. Clin Exp Obstet Gynecol. 2014;41 (1):67-71. PMID: 24707687
2. McKechnie L, Vasudevan C, Levene M. Neonatal outcome of congenital ventriculomegaly. Semin Fetal Neonatal Med. 2012;17(5):301-307. PMID: 22819382 DOI:10.1016/j.siny.2012.06.001
3. Kelly EN, Allen VM, Seaward G, et al. Mild ventriculomegaly in the fetus, natural history, associated findings and outcome of isolated mild ventriculomegaly: a literature review. Prenat Diagn. 2001;21(8):697-700. PMID: 11536274 DOI:10.1002/pd.138
4. McKechnie L, Vasudevan C, Levene M. Neonatal outcome of congenital ventriculomegaly. Semin Fetal Neonatal Med. 2012;17(5):301-307. PMID: 22819382 DOI:10.1016/j.siny.2012.06.001
5. Pisapia JM, Akbari H, Rozycki M, et al. Use of Fetal MRI and Machine Learning to Predict CSF Diversion in Fetal Ventriculomegal. JAMA Pediatr. 2018;172(2):128-135. PMID: 29255892 DOI:10.1001/jamapediatrics.2017.3993
6. Shi W, Yan GH, Li YM, et al. Fetal brain age estimation and anomaly detection using attention-based deep ensembles with uncertainty. Neuroimage. 2020;223:117316. PMID: 32890745 DOI:10.1016/j.neuroimage.2020.117316
7. Pisapia JM, Rozycki M, Akbari F, et al. Correlations of atrial diameter and frontooccipital horn ratio with ventricle size in fetal ventriculomegaly. J Neurosurg Pediatr. 2017;19(3):300-306. PMID: 28059680 DOI: 10.3171/2016.9.PEDS16210.
8. Yushkevich PA, Piven J, Hazlett HC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31(3):1116-1128. DOI:10.1016/j.neuroimage.2006.01.015
Figures
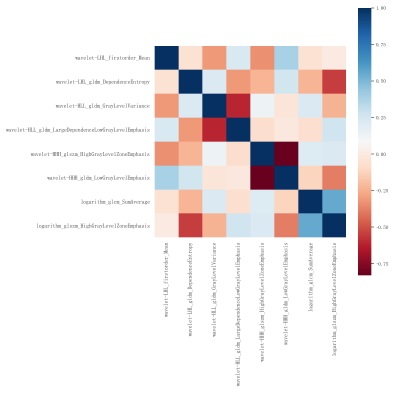
Figure 1. Heat maps show the distribution of the top 8 imaging features of the occipital lobe white matter on the dilated side, discriminating between the FV resolved group and the FV stabilized group among the training and test sets.
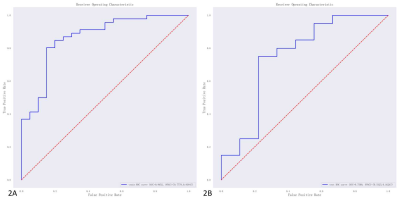
Figure 2. Receiver operating characteristic (ROC) curves of the occipital white matter radiomics on the dilated side of the training (2A) and test sets (2B) computed by using the Gaussian NB method. The AUC values of the training and test sets were 0.8652 (95%CI = 0.7778~0.9384) and 0.7500 (95%CI = 0.5325~0.9226), respectively.
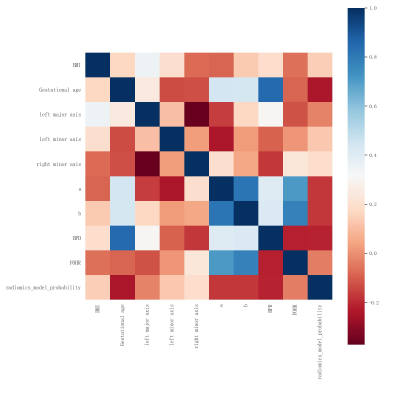
Figure 3. Heat maps of the most predictive radiomics features of white matter, maternal BMI, GA, and 2D diameters of the lateral ventricle discriminating between the FV resolved group and FV stabilized group among the training and test sets. BMI indictates maternal body mass index; GA, fetus gestational age; AD, atrial diameter of the lateral ventricles; a, the mean of the maximum frontal; b, the mean of occipital horn diameters; BPD, the biparietal diameter; FOHR, the fronto-occipital horn ratio; the major and minor axis lengths of each occipital horn; FOHR = [(a + b)/2BPD].
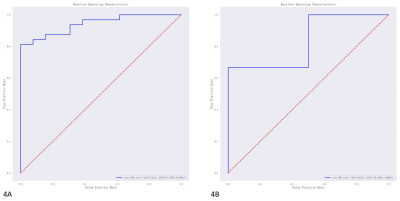
Figure 4. ROC curves of the combination of white matter radiomics, maternal BMI, GA, and 2D diameters of the lateral ventricle of the training (4A) and test sets (4B). The AUC values of the training and test sets were 0.9423 (95%CI = 0.8857~0.9862) and 0.8333 (95%CI = 0.5000~1.000), respectively.