3712
SNR enhancement in rapid high b-value prostate single-shot DW-EPI utilizing deep learning constrained Compressed SENSE reconstruction1Philips Japan, Tokyo, Japan, 2Tokyo Metropolitan Police Hospital, Tokyo, Japan, 3Philips Healthcare, Best, Netherlands, 4Philips GmbH Market DACH, Hamburg, Germany
Synopsis
DWI is a key component of the prostate MRI examination, but current prostate DWI images acquired with high b-value DWI using SENSE often suffer from increased noise artifacts. We propose to utilize a deep learning constrained Compressed SENSE (CS-AI) for reducing the noise artifacts in single-shot DW-EPI images. CS-AI DWI clearly reduces noise-like artifacts, boosts the overall SNR and significantly improves the accuracy and robustness of ADC values in rapid high b-value prostate DWI compared with conventional SENSE- and CS-DW-EPI, without any penalty for scan parameters.
PURPOSE
Diffusion-weighted imaging (DWI), including an apparent diffusion coefficient (ADC) map and high b-value images, is a key component of the prostate multi-parametric MRI exam1. High b-value diffusion imaging, with typical b-values of 2000 s/mm2 is advantageous in detection and assessment of prostate cancer2-4. With increasing b-value, the signal-to-noise ratio (SNR) decreases, so that the achieving adequate SNR is crucial for clinically acceptable image quality. In fact, high b-value DWI with SENSE (sensitivity encoding) often suffers from increased noise-like artifacts on the center of the images due to the high geometry factor when large acceleration factors are used with respect to the coil geometry characteristics5,6. To solve the problem, DW-EPI utilizing Compressed SENSE7 reconstruction framework (CS-EPI) has been introduced8,9. CS-EPI clearly reduced noise-like artifacts and significantly improves the accuracy and robustness of ADC values in small-FOV high b-value prostate DWI without any penalty for scan parameters9.Recently, integrating artificial intelligence (AI) into the Compressed SENSE reconstruction (CS-AI), based on Adaptive-CS-Net10,11, has been introduced and CS-AI dramatically reduced noise artifacts and significantly improved the accuracy and robustness of T2 values in submillimeter high-resolution prostate T2 mapping12. We hypothesize that the CS-AI reconstruction can further boost the SNR of high b-value prostate DWI. In this study, we attempt to utilize the CS-AI framework for reducing the noise artifacts in single-shot DW-EPI images. The purpose of this study is to demonstrate the clinical usefulness of CS-AI in prostate DWI with b-value of 2000 s/mm2 in patients, compared to conventional SENSE and CS-DWI.
METHODS
A total of 14 patients with suspected prostate cancer were examined on a 3.0T whole-body clinical system (Ingenia Elition X, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects.CS-AI DWI is based on single-shot DW-EPI acquisition. We did not modify its sampling pattern and applied the CS-AI framework for reconstruction. The CS-AI model used in this study is the extension of the Adaptive-CS-Net algorithm. In CS-AI, the iterative optimization procedure in the C-SENSE reconstruction chain is unrolled for a fixed number of Unet type of blocks. The model was trained on more than 700,000 images, including 2D and 3D data, and multiple contrasts and anatomical areas.
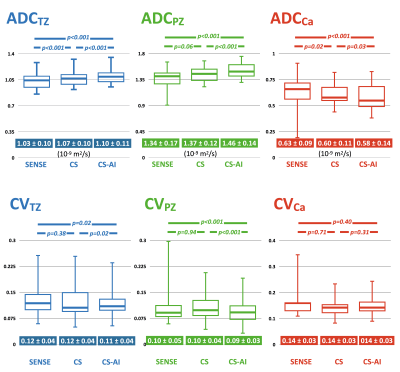
CS-AI-DWI images were compared with conventional SENSE and CS-DWI images for image quality, especially for the reduction of image noise. To demonstrate the improvement of the robustness of the ADC values thanks to the CS-AI noise reduction, we compared ADC values with SENSE and CS scans with exactly the same scan parameters. ROIs were placed on left and right transition zones (TZ), left and right peripheral zones (PZ) and prostate cancer (Ca, a total of 14 lesions). The average ADCs of TZ, PZ and Ca were used for comparison among SENSE, CS and CS-AI. Furthermore, we calculated the Coefficient of Variation (CV) of ADC values inside the ROIs in respective patients as follows: CV = SDADC / AverageADC, to evaluate the consistency of ADC values. Respective ADC and CV values were assessed by using one-way repeated measures analysis of variance (ANOVA) and the post-hoc Tukey test.
Imaging parameters for DWI were as follows: voxel size=2.5*3*3mm3, FOV=320*320mm, 20slices, b-value=0 and 2000s/mm2, TR=3528ms, TE=76ms, SENSE/C-SENSE acceleration factor=2.0, NSA=7 (SENSE) and 5 (CS/CS-AI), and total acquisition time=1min48s (SENSE) and 1min17s (CS/CS-AI). We shortened the scan time with CS/CS-AI about 30% (1:48 -> 1:17) compared with conventional SENSE in this study.
RESULTS and DISCUSSION
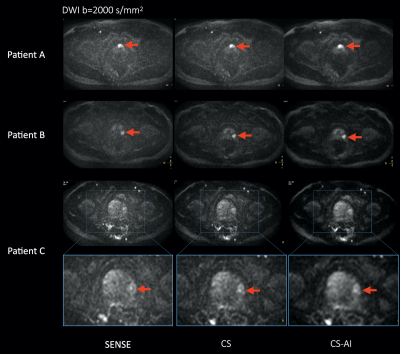
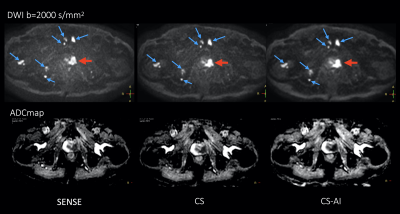
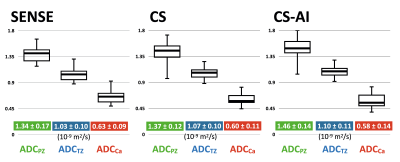
Fig.1 shows representative images of three patients with prostate cancer. CS reduced the noise in the center of the SENSE-DWI images, and CS-AI even further cleaned up the noise compared to CS. Fig. 2 shows another patient’s images of b=2000s/mm2 DWI and corresponding ADC maps. Prostate cancer (red arrow) and multiple bone metastases (blue arrows) in CS-AI images were more conspicuous compared with SENSE and CS.Fig.3 shows the ADC and CV values of TZ, PZ and cancer. The ADC values with CS-AI indicated higher values in TZ and PZ. On the other hand, CS-AI indicated lower cancer ADC than others. These differences were most likely due to the presence of severe noise over the prostate and CS-AI clearly removed such noise. Furthermore, CV values of CS-AI were lower than those of SENSE/CS. It indicated that CS-AI can provide more accurate ADC values with high reproducibility and robustness. Fig.4 shows the ADC comparison among PZ, TZ and cancer in respective acceleration techniques. CS-AI clearly discriminated in ADC values between TZ and cancer without overlapping. Although further clinical investigation is needed, CS-AI might be clinically useful in assessment of prostate cancer in more detail.
CONCLUSION
CS-AI DWI clearly reduces the noise-band artifacts, boosts the overall image SNR and significantly improves the accuracy and robustness of ADC values in rapid high b-value prostate DWI compared with conventional SENSE- and CS-DW-EPI, without any penalty for scan parameters. This technique may be helpful to further assess prostate cancer pathology.Acknowledgements
No acknowledgement found.References
1. Weinreb JC, et al. PI-RADS prostate imaging–reporting and data system: 2015, version 2. European Urology 2016;69:16-40.
2. Wang X, et al. High-b-value diffusion-weighted MRI for the detection of prostate cancer at 3 T. Clin Radiol. 2014;69:1165-70.
3. Kim CK, et al. High-b-value diffusion-weighted imaging at 3 T to detect prostate cancer: comparisons between b values of 1,000 and 2,000 s/mm2. AJR Am J Roentgenol. 2010 Jan;194(1):W33-7. doi: 10.2214/AJR.09.3004.
4. Katahira K, et al. Ultra-high-b-value diffusion-weighted MR imaging for the detection of prostate cancer: evaluation in 201 cases with histopathological correlation. Eur Radiol. 2011 Jan;21(1):188-96. oi: 10.1007/s00330-010-1883-7.
5. Patricia N, et al. Parallel Imaging Artifacts in Body Magnetic Resonance Imaging. Can Assoc Radiol J. 2009;60: 91–98.
6. Yanasak NE, et al. MR imaging artifacts and parallel imaging techniques with calibration scanning: a new twist on old problems. Radiographics. 2014;34:532-48.
7. Geerts-Ossevoort L, et al. Compressed SENSE Speed done right. Every time. The Netherlands: Philips Healthcare; 2018 Jan. Report No: 4522 991 31821. https://www.philips.de/content/dam/b2bhc/de/resourcecatalog/landingpages/ingeniaelition/White_Paper_Compressed_SENSE-opt.pdf
8. Kaga T, et al. Diffusion-weighted imaging of the abdomen using echo planar imaging with compressed SENSE: Feasibility, image quality, and ADC value evaluation. Eur J Radiol. 2021 Sep;142:109889. doi: 10.1016/j.ejrad.2021.109889.
9. Yoneyama M, et al. Noise Reduction in Prostate Single-Shot DW-EPI utilizing Compressed SENSE Framework. Proc Intl Soc Mag Reson Med. 2019:1634.
10. Pezzotti N, et al. An Adaptive Intelligence Algorithm for Undersampled Knee MRI Reconstruction. IEEE Access. 2020;8:204825-204838.
11. Pezzotti N, et al. Adaptive-CS-Net: FastMRI with Adaptive Intelligence. arxiv. 2019;(NeurIPS).
12. Yoneyama M, et al. Rapid submillimeter high-resolution prostate T2 mapping with a deep learning constrained Compressed SENSE reconstruction. Proc Intl Soc Mag Reson Med. 2021:4117.
Figures